What Is a Dural Leak?
Alila Medical Media/Shutterstock
We’ve seen many patients through the years with chronic dural leaks. What is that? How is a dural leak diagnosed? Can it be treated? Let’s dig in.
What Is a Dural Leak?
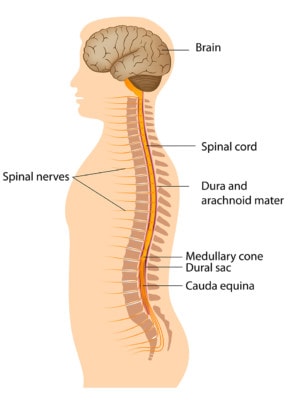
The dura is the covering of the spinal cord and nerve roots. It forms a sac of sorts that contains cerebrospinal fluid (CSF), or the liquid that bathes the brain and spinal cord. If that sac gets a hole in it, it’s called a dural leak (1). While some of these are big affairs related to trauma where a large hole or tear occurs, many are small holes with leaks that are often very slow, drip by drip. It’s the latter type that’s the focus of this article.
One of the things to understand about a dural leak is that the body is constantly making CSF at a rate of about half a liter a day (2). Hence, the patient gets symptoms when the amount of CSF leaking out per unit time exceeds the amount being made. Those symptoms come from a lack of pressure in the dural sac (CSF pressure), which can cause the brain to hang low in the skull and put pressure on critical brain tissue and nerves. This situation also provides very poor protection for the brain in the skull as you move around, as one of the purposes of the CSF is to protect the brain as you move.
What Are Dural Leak Symptoms?
The symptoms of a dural leak are pretty specific in some ways and general in others (3). For example, a specific symptom of a dural leak is a severe headache that presents itself when the patient is upright, but that promptly resolves when the patient is lying flat. That happens because the rate of the leak gets faster when the fluid pressure increases on standing (due to gravity) and then the pace slows when lying down. Other dural leak symptoms like dizziness or neck pain or ringing in the ears can also be positional.
The general part of the dural leak symptoms are the symptoms themselves like a headache. Meaning there are dozens of medical problems that can also cause headaches. Hence, sorting through all of those may be needed to make sure the patient has a dural leak causing their headache.
What Causes a Dural Leak?
A tear in the dura can happen due to trauma like a car crash. In addition, patients with super-stretchy ligaments (Ehlers Danlos Syndrome) are also at risk for spontaneous leaks (that aren’t related to trauma) (4). Other common causes include a lumbar puncture, sinus or spinal surgery, or a spinal injection procedure (like an epidural).
How Do You Diagnose a Dural Leak?
This is where things get tough. There are a number of diagnostic imaging tests that can be done like MRI myelography or Radionucleotide Cisternograthy, but the reality is that if you have a slow leak these tests have a very high false-negative rate (5). Meaning that a negative test can be called by the radiologist when there is a slow leak. So while they may be worth trying, if you have the symptoms of a dural leak despite a negative test, that doesn’t rule out a dural leak.
Another method to try to diagnose a dural leak is CSF pressure monitoring (6). This means sticking a needle or catheter into the dura and measuring the pressure. If the pressure is low, this is called intracranial hypotension and this can be caused by a dural leak (among other things). The problem here is that we’re trying to find if there is a hole in the dura by making another hole in the dura (to insert the measurement device).
In my clinical experience, what’s the best way to rule out a dural leak? A blood patch. That’s a treatment where your blood is injected around the dura (epidural) using x-ray guidance. The blood clots and forms a physical barrier for the leak. The platelets in the blood can also help initiate some healing of the tear or hole. These are commonly performed by region. For example the whole lumbar or whole thoracic spine. If the patient’s symptoms go away, then we know that that specific region of the spine is where the leak is located.
Will a Dural Leak Heal on Its Own?
If the hole in the dural is small, like from an epidural injection, it may heal on its own over a few days to a week. If the problems persist longer than that, or if they are more severe, the dural leak may need to be treated.
How Is a Dural Leak Treated?
The first-line treatment for an acute spinal leak caused by a small hole (like an epidural) is a blood patch. Fibrin glue can also be injected when a more chronic dural leak is the issue (7). This is made from blood and sets up with the consistency of rubber cement. Surgery to repair larger holes can also be accomplished, but for smaller holes that are hard to identify, finding the right spot may be hard to determine.
We’ve been using newer dural leak treatments like platelet-rich plasma (PRP) and lysate (PL) for years now (see video below for more information on these blood products). These often help in patients who have failed other treatments. PRP and PL contain concentrated platelets or growth factors injected like a blood patch, but with more healing power. Below I’ll cover a patient history of this type of treatment.
Nex Gen Dural Leak Treatment
Susanna is a 72-year-old woman who was in a car crash at the age of 60. In 2018 she began to get headaches that she thought were sinus related, but an ENT physician ruled that out. She eventually underwent an MRI Myelogram which showed a possible slow dural leak and underwent a blood patch of that area at Cedar-Sinai, which failed to help her pain. When I saw her in March of 2020, she was suffering from headaches, nausea, and fatigue, all brought on by being upright and relieved by laying down.
Given that the most common place for a dural leak is actually in the lumbar spine (because there is more pressure from gravity on the CSF there), she underwent a blood patch with platelet lysate from the sacrum (caudal epidural) to T12. That’s about 7-9 different fluoroscopically guided injection procedures, so IV anesthesia medication was used during the procedure. Again, platelet lysate was used because it contains more healing growth factors than a blood patch or fibrin glue. I spoke to the patient today about another issue and followed up on this procedure. Within a few weeks of the injection back in march of 2020, all dural leak symptoms disappeared and haven’t returned 15 months later. This report is consistent with healing of the tear.
The upshot? Dural leaks can be disabling. Finding one on imaging can be hit or miss, so defining where they live is best accomplished with blood patching. Getting them to heal, in my experience, can usually be done by using the regenerative properties of the patient’s own platelets.
____________________________
References:
(1) Gandhi J, DiMatteo A, Joshi G, Smith NL, Khan SA. Cerebrospinal fluid leaks secondary to dural tears: a review of etiology, clinical evaluation, and management. Int J Neurosci. 2020 May 13:1-7. doi: 10.1080/00207454.2020.1751625. Epub ahead of print. PMID: 32242448.
(2) Sakka L, Coll G, Chazal J. Anatomy and physiology of cerebrospinal fluid. Eur Ann Otorhinolaryngol Head Neck Dis. 2011 Dec;128(6):309-16. doi: 10.1016/j.anorl.2011.03.002. Epub 2011 Nov 18. PMID: 22100360.
(3) Bosacco SJ, Gardner MJ, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat Res. 2001 Aug;(389):238-47. doi: 10.1097/00003086-200108000-00033. PMID: 11501817.
(4) Reinstein E, Pariani M, Bannykh S, Rimoin DL, Schievink WI. Connective tissue spectrum abnormalities associated with spontaneous cerebrospinal fluid leaks: a prospective study. Eur J Hum Genet. 2013;21(4):386-390. doi:10.1038/ejhg.2012.191
(5) Schievink WI, Meyer FB, Atkinson JL, Mokri B. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. J Neurosurg. 1996 Apr;84(4):598-605. doi: 10.3171/jns.1996.84.4.0598. PMID: 8613851.
(6) Craven C, Toma AK, Khan AA, Watkins LD. The role of ICP monitoring in patients with persistent cerebrospinal fluid leak following spinal surgery: a case series. Acta Neurochir (Wien). 2016 Sep;158(9):1813-9. doi: 10.1007/s00701-016-2882-5. Epub 2016 Jul 8. PMID: 27393191.
(7) Siedentop KH, O’Grady K, Park JJ, Bhattacharya T, Sanchez B. Fibrin sealant for treatment of cerebrospinal fluid leaks. Am J Otol. 1999 Nov;20(6):777-80. PMID: 10565724.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
