How Do You Explain Interventional Orthopedics?
This past week an ex-college football coach visited our Colorado facility. I struggled for a few minutes to explain how different interventional orthopedics is from what he knew of orthopedic stem cell injections. This is a video version of what I drew on the dry-erase board for him, and since this is often a tough thing to explain to patients and physicians alike, I decided to use it on the blog this morning.
How Is What We Do Every Day Very Different from What 99% of Clinics Can Offer?
Our fellow from last year, Dr. Bashir, decided to stay on in Colorado for a year as an attending physician before he ventured down to Miami to open a Regenexx site. As colleagues, we often go back and forth on new interventional orthopedics procedures with neither of us taking a minute to understand that what we’re discussing is way over the skill levels of 99% of the physicians who say they can do an orthopedic stem cell injection.
As an example, not satisfied with the way we usually teach to precisely place stem cells into an injured shoulder labrum (or wanting to develop his own techniques now that he’s mastered ours), Dr. Bashir has been working on a new ultrasound and fluoroscopy-based method. He showed me a very nice fluoro image this week demonstrating great contrast flow in various parts of the labrum. As I looked at the image, I thought to myself that only about 100 US physicians can even perform the original procedure, and now we’re working on an improvement?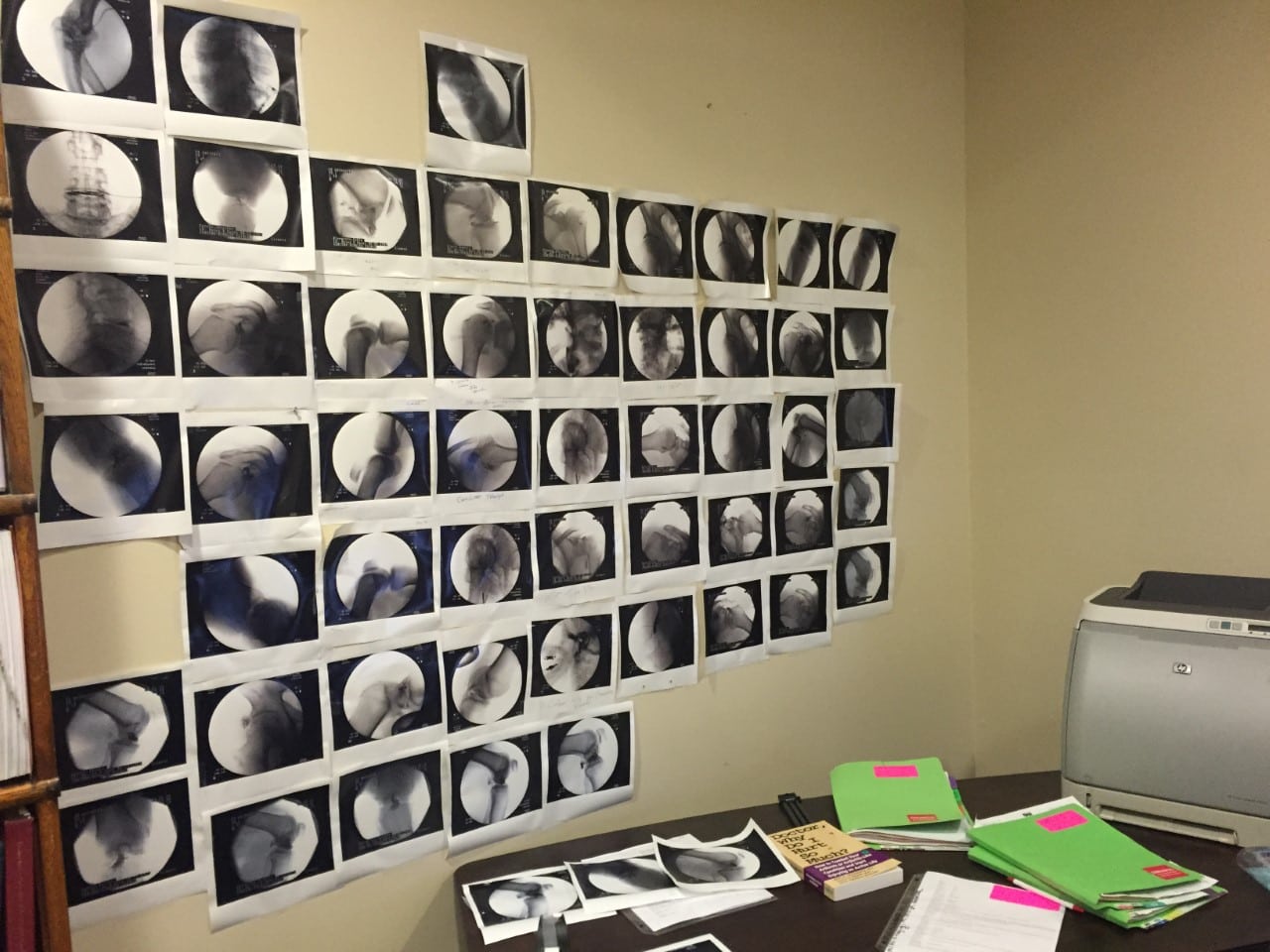
To the right is what I call, “Bashir’s Interventional Orthopedics Wall of Fame.” Each of these images represents a different precise image-guided procedure we perform that was a best-case example. These live in Dr. Bashir’s office, and they are a constant reminder to me that we have an entire generation of physicians to educate on this new approach to orthopedics.
Can’t My Doctor Who Uses Ultrasound or Fluoroscopy Do This?
The old ball coach had an orthopedic injection down in Mexico this week. As he told me that the Mexican doctor used fluoroscopy, I used a dry-erase board to explain the differences between what he had received and what we do every day at Regenexx.
The procedure he had in Mexico was a simple intra-articular joint injection using fluoroscopy (real time X-ray). While this was better than a blind joint injection, stem cells aren’t magic, and if his problem had been in the shoulder labrum, rotator cuff, or ligaments, the procedure would have likely failed because the doctor didn’t have the knowledge of how to inject those structures. Lucky for the ball coach, his pain was due to arthritis in the main shoulder joint, so placing cells there helped his shoulder.
As we spoke, I tried to have him understand that while an orthopedic surgeon may be very experienced in surgically reforming or stabilizing tissue, that surgeon has little education in advanced regenerative-medicine injections using imaging guidance. In addition, he or she doesn’t posses the skill set to place cells into very specific joint structures without surgery. However, neither do the vast majority of the family-practice sports-medicine physicians, physical-medicine doctors, interventional radiologists, and interventional spine specialists.
As a concrete example, let’s focus on the knee. We speak to a huge number of seemingly qualified physicians each year who want to join our expanding medical group. Regrettably, most are only familiar with one type of knee injection procedure. In this injection, the physician first identifies the main knee joint space above the kneecap with ultrasound. He or she then injects platelets or stem cells. That’s the extent of their knowledge. If they take a weekend course in ultrasound knee injections, they may be taught how to also inject the patellar and quadriceps tendons.
Here are the structures that we at Regenexx routinely inject:
- Meniscus
- Patellar tendon
- Quadriceps tendon
- Pes tendons
- Patellar bone
- Femur bone
- Tibia bone
- LCL
- MCL
- ACL
- ALL
- PCL
- Specific joint areas, such as patellofemoral
- Coronal ligaments
- POL
- MPFL
This is just the knee! There’s a list like this for each body part. Each of these procedures takes awhile to understand and master, so a physician could spend months to years becoming an expert in these procedures, just in the knee.
Based on asking physicians to fill out what we call our “CORE Skills” checklist, if we put them in a room with a cadaver knee and ultrasound and fluoroscopy, only about 1% of US physicians and surgeons who say they can perform orthopedic PRP or stem cell injections could perform all of the above procedures. Maybe a few percent more could do some of them, and 95% of the doctors would look at us like we we’re speaking Chinese and fumble through almost all of them or have the courage to say, “I don’t know” (which is a tough thing to say for many doctors).
The Interventional Orthopedics Foundation to the Rescue
Some of the procedures in the list above and for other joints were invented by our clinic in Colorado, and some were pioneered elsewhere. While we do a great job of heavily screening physicians based on their image-guided-injection knowledge and then training them on how to perform these procedures, that’s still a small group. If interventional orthopedics is ever going to grow as a separate medical specialty, these and other procedures have to be taught to many other qualified physicians. Hence, this year, we agreed to assist the Interventional Orthopedics Foundation (a 501c3 nonprofit we helped start) in creating structured course work to ensure that every qualified doctor could understand how best to place orthobiologics into these specific areas of need.
First, why train the competition? It’s needed to serve a bigger need—the improvement of patient care through a shift away from elective and invasive orthopedic surgery to less-invasive interventional orthopedics. That’s a goal bigger than one medical group, like Regenexx. In addition, 10,000 well-trained minds all working on how that future unfolds is simply better than 30–100. Second, aren’t there already courses that doctors can take to learn these procedures? While there are a few courses that offer a few of these injections, there are none that offer all of them. In addition, all of the courses are for profit, so their motives are usually focused around selling products. While I have nothing against selling products, physicians need a place where they can come and learn that’s simply focused on the procedures. For example, how best can I get a needle or other similarly sized tool into a 1 mm by 1 mm spot using fluoroscopy or ultrasound without having to worry about being sold something? A place where the medicine drives the conversation, not the sales discussion. So a 501c3 nonprofit was the perfect vehicle for that type of education. What if your doctor doesn’t know how to perform these advanced procedures? Then he or she can now remedy that situation through structured course work through a nonprofit.
The upshot? A chance meeting with an old ball coach prompted yet another way for me to help explain interventional orthopedics and why it’s very, very different from what’s being done out there in 2016. Hopefully by 2030 or so, through nonprofits, like the Interventional Orthopedics Foundation, every qualified physician in the world who wants to be able to get stem cells into the shoulder superior labral anchor, the knee ACL, or a hip AVN bone lesion will be able to do that like it’s second nature. Since that’s about when I’ll be retiring, that would be a great retirement present along with my gold watch!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
