Fluoroscopy vs Ultrasound for Orthobiologic Spine Procedures
One of the more interesting debates from the past 5 years has been the use of fluoroscopy versus ultrasound guidance in advanced spinal injections. This one gets physicians emotional, as many believe that they can now offer patients the same type of injections using only an ultrasound machine when compared to x-ray guidance. So let’s dive into the controversy.
What We’re Not Discussing
What we’re not discussing is the use of ultrasound to perform simple injections like spinal ligaments or muscles. There is little doubt for me that you can use this technology to perform those kinds of injections and that you can do that with high levels of accuracy.
What We Are Discussing
Deeper spinal injections like transforaminal epidurals (TF epidurals) are what we’re discussing. Today, to keep this simple, I’ll focus on TF epidurals. This is an injection that is deep around the exiting nerve in the foramen, epidural, and up around the disc where the spinal nerve gets irritated.
The Advantages and Disadvantages of Fluoroscopy vs. Ultrasound
Each of these technologies has its advantages and disadvantages, which is why IMHO any advanced provider using orthobiologics needs to be adept at using both. Here is the Reader’s Digest:
Fluoroscopy
Advantages:
- Can see through bone
- Can localize the needle in deeper structures with more accuracy
- Can be paired with other technologies like Digital Subtraction Angiography (DSA) to alert the doctor to an injection inside a small artery that shouldn’t be injected
Disadvantages:
- Uses ionizing radiation
- Can’t see soft-tissues
- More expensive than ultrasound by about 2-3X
Ultrasound
Advantages:
- Can see soft tissues
- Doesn’t use ionizing radiation
- Less expensive than fluoroscopy
Disadvantages:
- Can’t see through bone
- Less accuracy in localizing the needle in deep structures
- Can’t accurately see all injections into small arteries
In summary, for superficial spine injections like ligaments, ultrasound is the way to go as it can see these soft tissues. On the other hand, deep spinal injections where the injectate can go behind bone are just not as accurate using ultrasound. Let’s go over that last point.
Deep Spinal injections Using Fluoroscopy and Ultrasound
So lets use these concepts where the rubber meets the road. We’ll look at an advanced specialized type of epidural called “transforaminal”. This is used when a disc bulge is irritating a spinal nerve. To treat this, the doctor can precisely inject an orthobiologic like platelet lysate around the nerve to get rid of the symptoms while the body takes care of repairing the disc bulge. In my experience, that’s a procedure that can help lots of patients avoid low back surgery.
Here’s what happens when the doctor uses fluoroscopy and injects radiographic contrast so the provider can see where the orthobiologic is going:
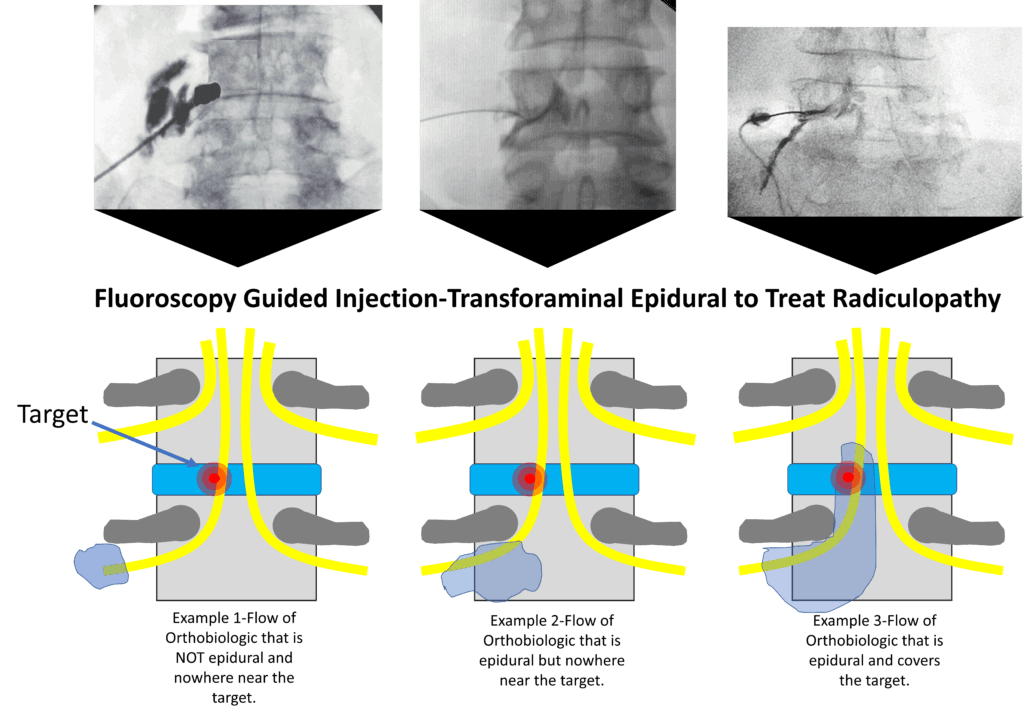
Note that in the lower images, the yellow represents the nerves and the target is shown in red. That’s the place where the disc bulge is irritating the descending nerve. Hence, the job of the doctor is to get the orthobiologic to that spot. However, regardless of how experienced the doctor is at these procedures, there are many times that the injection only stays local as in the left-most images. That light purple blob never makes it to the target in Example 1. When that happens the doctor needs to adjust the needle and try again. That may result in what you see in example 2, where the orthobiologic gets into the epidural space, but doesn’t make it to the target. The doctor can see this easily on the screen because the doctor can see through the bone. Finally, after the doctor adjusts the needle again, he sees what’s shown in example 3, where the injectate makes it epidural all the way to the target. Again, this can be easily seen because the doctor can see through the bone, and for the most part, what’s being injected is being shielded by bone.
How often do examples 1 and 2 happen, even in experienced hands? About 1/4 to half of the time.
How about using ultrasound? Let’s look at that below:
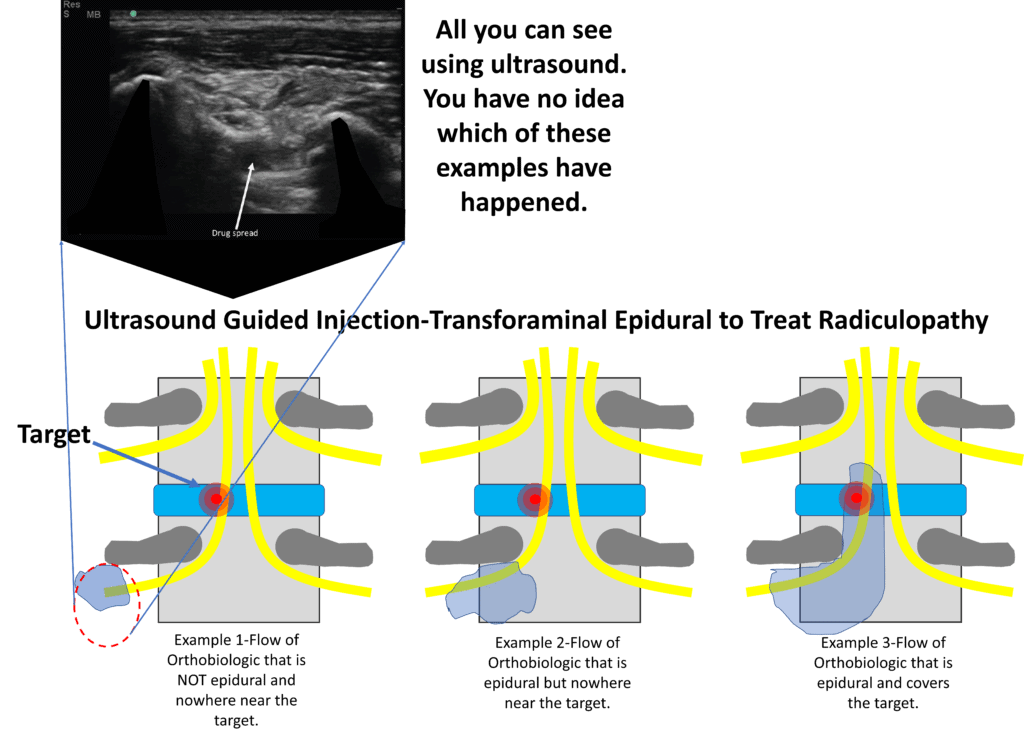
Note that in order to inject “transforaminal” the doctor can see the foramen (where the nerve lives) using ultrasound (that is if the patient is on the thinner side, this becomes much harder if the patient is significantly overweight). However, all the doctor can see is example 1, that the orthobiologic made it around the nerve. Because ultrasound can’t see through bone and the rest of the course of the injectate is under bone, the doctor has no ability to determine if he’s dealing with an injectate that made it to the target. Which is the big issue here.
Again to review, using ultrasound:
- The accuracy declines rapidly as the patient’s weight increases. With obesity rates reaching more than 50% in many areas, that’s a big issue.
- Even if the patient is thinner, ultrasound can’t see through bone, so unlike the fluoroscopy epidural, the doctor won’t usually be able to determine if the orthobiologic made it to the target where the disc meets the nerve.
Can You Perform Advanced Spinal Injections Like This Using Ultrasound?
Here’s how I put this to patients. Can I do this procedure using ultrasound? Yes, I can. However, I can’t guarantee that the procedure is done well in the same way that can be guaranteed using fluoroscopy.
Why Would All Providers Advertising Advanced Spinal Procedures Not Use Fluoroscopy?
That’s a good question. However, in medicine, oftentimes physician convenience dictates treatment options. Fluoroscopy is more expensive, so sometimes that drives the decision. Other times these things are determined by hospital turf battles. For example, in many hospital settings, fluoroscopy machines can only be easily accessed by certain provider types.
Would I Allow a Transforaminal Injection to Be Performed on My Back Using Only Ultrasound?
NO. Not only do we have the issue above, but there’s another more dangerous problem. If the doctor places the needle too deeply, the medication can be injected “intrathecal” or inside the dura (the covering of the spinal cord and nerve roots). Medication travels rapidly upwards in that space, even if small amounts are used. That means that just 5-10 cc of an anesthetic injected in the low back inadvertently injected intrathecal can, in some patients, cause breathing to stop by numbing out the breathing center in the upper neck. In addition, this will cause a dural leak. With fluoroscopy, this can be easily detected and the needle repositioned, with ultrasound it can’t be easily detected.
There’s another danger zone issue, which is the radicular artery. This small artery supplies the spinal cord. If it’s inadvertently injected with something like PRP, that can cause a spinal cord stroke through a blood clot blocking that blood supply. Again, this could be easily seen with fluoroscopy with DSA and the needle moved with no harm no foul. With ultrasound, this is much harder to detect.
The upshot? This blog will likely aggravate many providers who have tried to add advanced spinal injections to their practices by only buying an ultrasound machine. However, it’s also critical that the patients who get these procedures understand that there are key differences in accuracy and safety between using fluoroscopy and ultrasound for deep spinal injection procedures.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
