Hip Arthroscopy Recovery? Unlikely If You’ve Lost Half of Your Hip Cartilage…
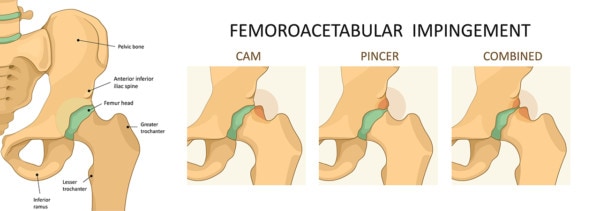
Hip arthroscopy has been all the rage lately. Many patients are getting offered this invasive surgery with various amounts of hip arthritis because their MRI shows evidence of impingement. Their focus is hip arthroscopy recovery, or a rapid return to their activities once they heal from surgery. However, a new paper published on registry data shows that many patients undergoing the surgery are less likely to recover if they have even moderate arthritis.
The paper looked at 153 patients who were older than 50 who had undergone hip arthroscopy for FAI (hip impingement) and the results of the 42% of them who were available for long-term follow-up. The analysis of the data showed that if the patient had at least 2 mm of cartilage remaining in the joint, they did well. However, if they had less than 2 mm of cartilage, they did poorly. While 2 mm of cartilage sounds like the patients who did poorly were “bone on bone”, that’s not really the case. The normal amount of cartilage in the human hip is only 3.61-3.63 mm. So if you had lost half of your hip cartilage, you did poorly with hip arthroscopy to treat impingement. Also to put this in perspective, what would the outcome have been if we just left this hip arthritis alone? For this study that’s tough to say, but we can use another large study to get a rough idea. A study in 2011 out of Iceland looked at the x-rays of nearly 3,000 hips and defined hip arthritis as having 2.5 mm of cartilage or less. Surprisingly, 11-28 years later, despite a socialized healthcare system, more than 4 in 5 patients with 2.5 mm of cartilage or less (arthritis) had not gotten a hip replacement! Patients with 2 mm or less of cartilage in this hip surgery study got a hip replacement about 2 in 5 times, more frequently than the study in Iceland. One could argue that this is because of their hip impingement, but since recent studies show that many patients with normal hips meet the definition of hip impingement on imaging, it’s a good bet that many of the patients in the Iceland study had impingement (or the bigger issue, dysplasia-a short hip socket).
Logika600/Shutterstock
Is Fixing Hip Impingement a Good Idea? Are Those Bone Spurs Preventing Arthritis?
The upshot? Most patients over age 50 who get a MRI for disabling hip pain and are later diagnosed with impingement have less than 2 mm of hip cartilage. Based on this study, those patients are not good candidates for hip arthroscopy. Despite this study, we continue to see many of these moderate arthritis patients operated to treat the impingement. In addition, since less than 2 in 10 patients in this general category never opt for a hip replacement naturally, one has to ask the question why 4 in 10 patients are opting for an early hip replacement after hip arthroscopy when the “impingement” has been removed surgically? Could it be that the bone spurs we’re removing are protective? Indeed, at least based on one well done study on hip impingement this seems to be the case. The bone spurs that surgeons believed were a cause of arthritis were actually protecting the joint from more arthritis. So should we remove these protective bone spurs? Not IMHO.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
