How a Bad Study Can Teach Us About PRP
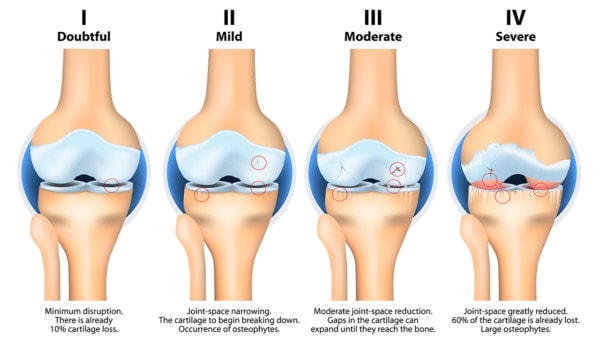
Stages of knee osteoarthritis. Designua/Shutterstock
Just because something gets published with a conclusion doesn’t mean that the research can support that conclusion. Case in point is a new study on knee radiofrequency versus PRP. Let’s dig in.
Knee Geniculate Nerve RFA
RFA stands for radiofrequency ablation. This procedure has become increasingly common to help the pain caused by moderate to severe knee arthritis where the patient is a candidate for knee replacement. There are geniculate nerves in the knee that surround the joint and carry the pain signals from the area. The general concept behind nerve ablation is that since the nerves carry pain signals from the arthritic joint, destroying the nerves through radiofrequency ablation should get rid of the arthritis pain (1).
Does this Knee RF Procedure Work?
While much of the research is made up of small studies, the answer is that there is some research showing that the procedure works (2-4). However, few high-level studies exist at this point. In addition, the one review of many studies showed that the procedure worked better for women than men and also helped knee pain, but not knee function.
The Downside of Frying Nerves
The reason that our practice in Colorado has avoided RFA of the knee geniculate nerves is that it’s destructive. Meaning it kills the nerves taking pain from the joint. Hence, the sensation from that joint will never be entirely normal once heat is used to kill the nerves, even if those nerves ultimately regenerate.
Regenerative vs a Destructive Procedure
PRP or platelet-rich plasma consists of concentrating the patient’s own healing platelets and injecting them into the knee joint. This works to help arthritis pain based on many, many published studies (5-21). That mechanism of action likely involves improving the knee’s ability to heal itself and downregulating inflammation. Hence, that effect is likely a net positive.
Knee geniculate nerve RFA works by destroying nerves, which is a net negative to the health of the joint. Hence, this is called a destructive procedure. To date, we have far more high-level research showing that PRP helps knee arthritis than exists for knee geniculate nerve RFA.
Does Knee RFA Work Better than PRP?
A new study was just published that tested knee RF versus PRP for knee arthritis patients (22). This randomized controlled trial reported:
“Pulsed radiofrequency of the genicular nerves can be considered superior to knee intraarticular platelet-rich plasma injection for sustained pain relief…”
However, there are a couple of caveats here once you read the fine print of the study.
Severe Knee Arthritis and PRP
The vast majority of studies that looked at the severity of knee arthritis and PRP efficacy concluded that while the procedure works well for less severe mild to moderate arthritis, it doesn’t work as well for moderate to severe arthritis. The problem with the above study is that they used moderate/severe arthritis patients who wouldn’t ordinarily be considered candidates for PRP.
In fact, the authors found what could have been predicted by using PRP in severely arthritic joints. It doesn’t last that long. Meaning they found that PRP provided good relief for 6 months and that was the same degree of relief as the RF treatment. After that, in the PRP group, the pain returned, If you use PRP injections in less severely arthritic joints, they usually show 1 year plus of relief.
In fact, based on the published research, the better orthobiologic treatment to compare RF to would have been bone marrow concentrate, which has been shown to work much better in moderate to severe knee arthritis patients (23-25).
Pulsed Vs. Cooled RF
This study also used pulsed radiofrequency, which is generally not covered as a benefit through insurance plans in the United States. What is mostly done here is thermal radiofrequency. The difference is that the former doesn’t hurt the nerve as much and the latter used her in the U/S. destroys the nerve.
The upshot? The reason why RF worked better here is that the authors used PRP in a situation where we would expect it not to work well. Hence, reading the fine print of a research study is critical!
___________________________________
References:
(1) Kidd VD, Strum SR, Strum DS, Shah J. Genicular Nerve Radiofrequency Ablation for Painful Knee Arthritis: The Why and the How. JBJS Essent Surg Tech. 2019;9(1):e10. Published 2019 Mar 13. doi:10.2106/JBJS.ST.18.00016
(2) El-Hakeim EH, Elawamy A, Kamel EZ, Goma SH, Gamal RM, Ghandour AM, Osman AM, Morsy KM. Fluoroscopic Guided Radiofrequency of Genicular Nerves for Pain Alleviation in Chronic Knee Osteoarthritis: A Single-Blind Randomized Controlled Trial. Pain Physician. 2018 Mar;21(2):169-177. https://www.ncbi.nlm.nih.gov/pubmed/29565947
(3) Gupta A, Huettner DP, Dukewich M. Comparative Effectiveness Review of Cooled Versus Pulsed Radiofrequency Ablation for the Treatment of Knee Osteoarthritis: A Systematic Review. Pain Physician. 2017 Mar;20(3):155-171. https://www.ncbi.nlm.nih.gov/pubmed/28339430
(4) Hong T, Wang H, Li G, Yao P, Ding Y. Systematic Review and Meta-Analysis of 12 Randomized Controlled Trials Evaluating the Efficacy of Invasive Radiofrequency Treatment for Knee Pain and Function. Biomed Res Int. 2019;2019:9037510. Published 2019 Jun 26. doi:10.1155/2019/9037510
(5) Uslu Güvendi E, Aşkin A, Güvendi G, Koçyiğit H. Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis. Arch Rheumatol. 2017;33(3):273–281. Published 2017 Nov 2. doi: 10.5606/ArchRheumatol.2018.6608
(6) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(7) Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee Osteoarthritis Injection Choices: Platelet- Rich Plasma (PRP) Versus Hyaluronic Acid (A one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. Published 2015 Jan 7. doi: 10.4137/CMAMD.S17894
(7) Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017;5(2):2325967116689386. Published 2017 Feb 13. doi: 10.1177/2325967116689386
(9) Montañez-Heredia E, Irízar S, Huertas PJ, et al. Intra-Articular Injections of Platelet-Rich Plasma versus Hyaluronic Acid in the Treatment of Osteoarthritic Knee Pain: A Randomized Clinical Trial in the Context of the Spanish National Health Care System. Int J Mol Sci. 2016;17(7):1064. Published 2016 Jul 2. doi: 10.3390/ijms17071064
(10) Lana JF, Weglein A, Sampson SE, et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016;12(2):69–78. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227106/
(10) Görmeli G, Görmeli CA, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017 Mar;25(3):958-965. doi: 10.1007/s00167-015-3705-6.
(12) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(13) Lin KY, Yang CC, Hsu CJ, Yeh ML, Renn JH. Intra-articular Injection of Platelet-Rich Plasma Is Superior to Hyaluronic Acid or Saline Solution in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized, Double-Blind, Triple-Parallel, Placebo-Controlled Clinical Trial. Arthroscopy. 2019 Jan;35(1):106-117. doi: 10.1016/j.arthro.2018.06.035.
(14) Huang Y, Liu X, Xu X, Liu J. Intra-articular injections of platelet-rich plasma, hyaluronic acid or corticosteroids for knee osteoarthritis : A prospective randomized controlled study. Orthopade. 2019 Mar;48(3):239-247. doi: 10.1007/s00132-018-03659-5.
(15) Di Martino A, Di Matteo B, Papio T, Tentoni F, Selleri F, Cenacchi A, Kon E, Filardo G. Platelet-Rich Plasma Versus Hyaluronic Acid Injections for the Treatment of Knee Osteoarthritis: Results at 5 Years of a Double-Blind, Randomized Controlled Trial. Am J Sports Med. 2019 Feb;47(2):347-354. doi: 10.1177/0363546518814532.
(16) Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018;16(3):2119–2125. doi: 10.3892/etm.2018.6412
(17) Buendía-López D, Medina-Quirós M, Fernández-Villacañas Marín MÁ. Clinical and radiographic comparison of a single LP-PRP injection, a single hyaluronic acid injection and daily NSAID administration with a 52-week follow-up: a randomized controlled trial. J Orthop Traumatol. 2018;19(1):3. Published 2018 Aug 20. doi: 10.1186/s10195-018-0501-3
(18) Su K, Bai Y, Wang J, Zhang H, Liu H, Ma S. Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis. Clin Rheumatol. 2018 May;37(5):1341-1350. doi: 10.1007/s10067-018-3985-6.
(19) Cole BJ, Karas V, Hussey K, Pilz K, Fortier LA. Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis. Am J Sports Med. 2017 Feb;45(2):339-346. doi: 10.1177/0363546516665809.
(20) Louis ML, Magalon J, Jouve E, Bornet CE, Mattei JC, Chagnaud C, Rochwerger A, Veran J3, Sabatier F. Growth Factors Levels Determine Efficacy of Platelets Rich Plasma Injection in Knee Osteoarthritis: A Randomized Double Blind Noninferiority Trial Compared With Viscosupplementation. Arthroscopy. 2018 May;34(5):1530-1540.e2. doi: 10.1016/j.arthro.2017.11.035.
(21) Lisi C, Perotti C, Scudeller L, Sammarchi L, Dametti F, Musella V, Di Natali G. Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A randomized controlled trial. Clin Rehabil. 2018 Mar;32(3):330-339. doi: 10.1177/0269215517724193
(22) Elawamy A, Kamel EZ, Mahran SA, Abdellatif H, Hassanien M. Efficacy of Genicular Nerve Radiofrequency Ablation Versus Intra-Articular Platelet Rich Plasma in Chronic Knee Osteoarthritis: A Single-Blind Randomized Clinical Trial. Pain Physician. 2021 Mar;24(2):127-134. PMID: 33740345.
(23) Centeno C, Sheinkop M, Dodson E, Stemper I, Williams C, Hyzy M, Ichim T, Freeman M. A specific protocol of autologous bone marrow concentrate and platelet products versus exercise therapy for symptomatic knee osteoarthritis: a randomized controlled trial with 2 year follow-up. J Transl Med. 2018 Dec 13;16(1):355. doi: 10.1186/s12967-018-1736-8. PMID: 30545387; PMCID: PMC6293635.
(24) Hernigou P, Bouthors C, Bastard C, Flouzat Lachaniette CH, Rouard H, Dubory A. Subchondral bone or intra-articular injection of bone marrow concentrate mesenchymal stem cells in bilateral knee osteoarthritis: what better postpone knee arthroplasty at fifteen years? A randomized study. Int Orthop. 2020 Jul 2. doi: 10.1007/s00264-020-04687-7. Epub ahead of print. PMID: 32617651.
(25) Hernigou P, Delambre J, Quiennec S, Poignard A. Human bone marrow mesenchymal stem cell injection in subchondral lesions of knee osteoarthritis: a prospective randomized study versus contralateral arthroplasty at a mean fifteen year follow-up. Int Orthop. 2020 Apr 23. doi: 10.1007/s00264-020-04571-4. Epub ahead of print. PMID: 32322943.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
