How Does the Body Stabilize the C1-C2 Joint? The Role of the Alar Ligament
Readers: Please excuse this in-depth and very dense discussion of the C1-C2 joint. I am preparing a large case series of PICL patients for publication and began writing this as a paper to be submitted for publication, but I decided that some of the rubber meets the road mechanism of the unique way that the C1-C2 joint is stabilized in rotation was worth sharing on my blog.
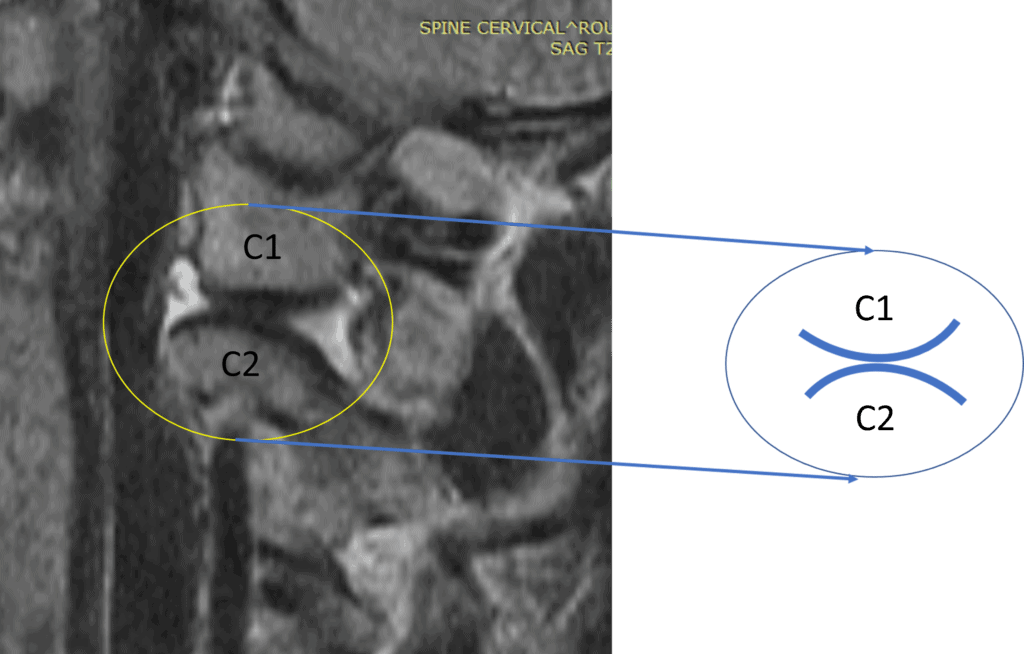
Upper cervical problems are surprisingly common, but this part of the spine rarely gets treated with regenerative medicine. In that area, one of the upper cervical facet joints that can cause headache pain is C1-C2. This joint can also become unstable, leading to manual adjustments that only provide temporary relief. Given that it’s a unique, inherently unstable, biconvex joint, how does that work? The alar ligament plays a critical role.
The C1-C2 Joint, Torticollis, and Headaches
Credit: Elsevier Complete Anatomy with Illustration by Author
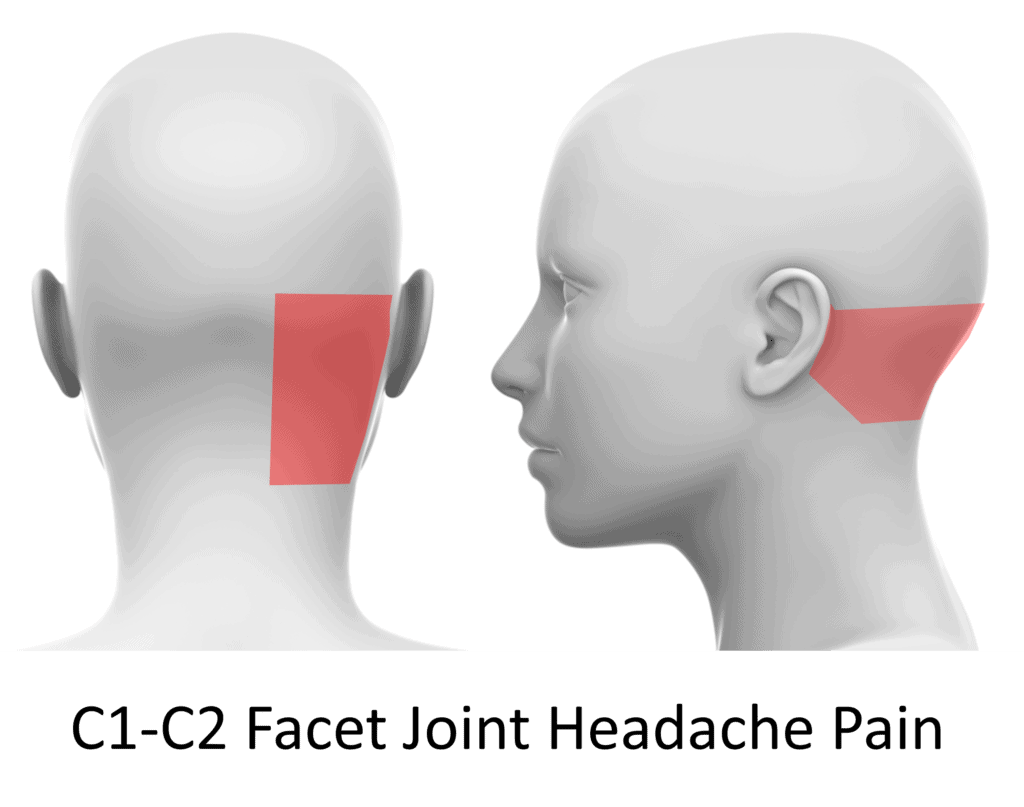
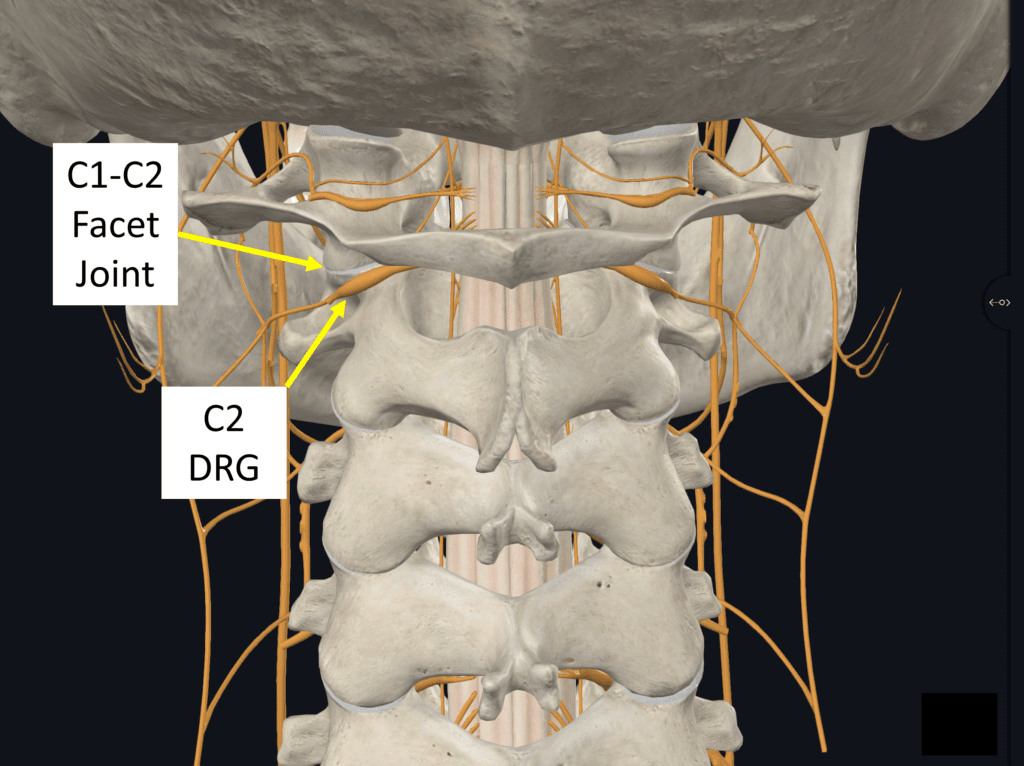
So why should you care about the C1-C2 facet joint? First, we know that it’s where about half of your neck rotation comes from, so that’s pretty critical (1). In addition, we also know that injuries to this joint can lead to torticollis, a problem where the muscles spasm, so the head is permanently turned to one side (2). We also know that the C1-C2 joint can cause headache pain (4). For example, in a study by Dwyer et al., pain from this joint referred to the back of the head at the base of the skull, as shown above (3). In addition to pain coming from the joint, the C2 dorsal root ganglion (DRG) lies just behind and below the joint, so if the joint is unstable, this nerve can be irritated:
Credit: Elsevier Complete Anatomy with Illustration by Author
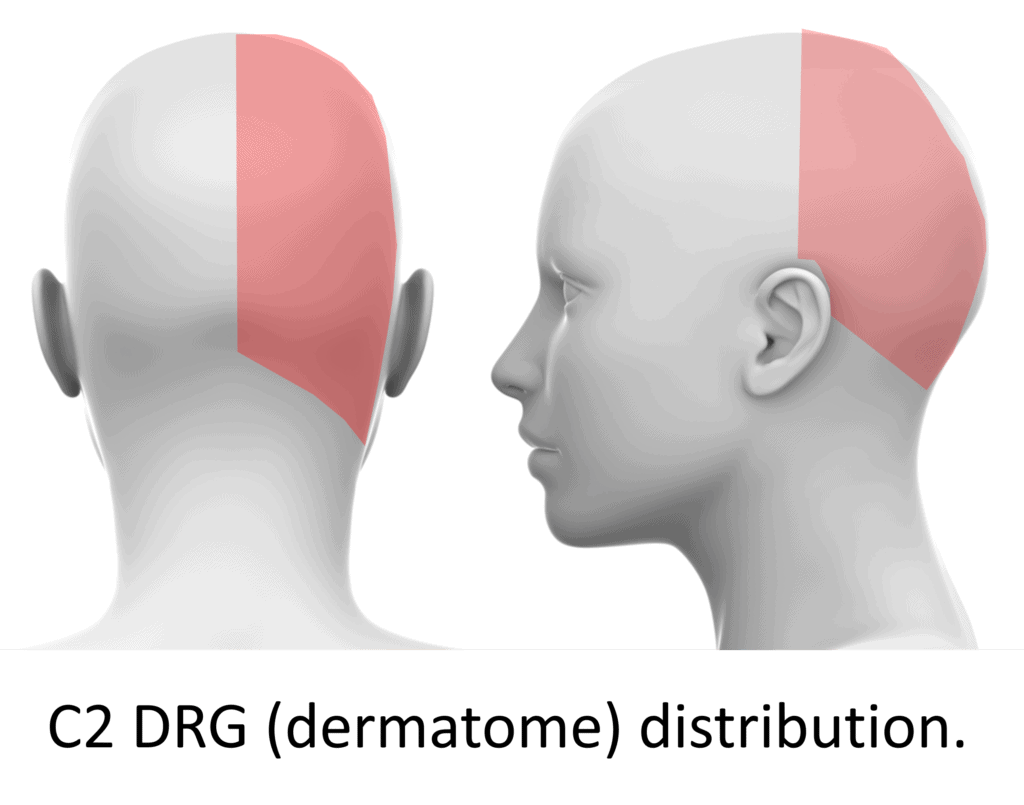
If the C2 DRG nerve is irritated by an unstable joint, pain, numbness, tingling, or decreased sensation can be felt in this distribution:
Credit: Shutterstock with Illustration by Author
The C2 DRG supplies the greater and lesser occipital nerves, so problems with this structure can mimic greater or lesser occipital neuralgia.
In summary, the C1-C2 joint can cause headaches or altered sensations in the head.
The Big Rotation Joint
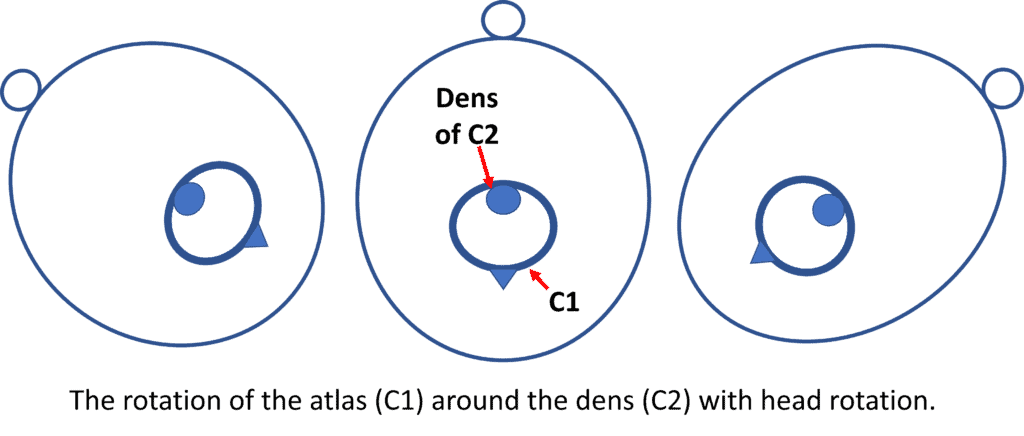
Each cervical facet joint level in the neck allows just a bit of rotation so that the C2-C7 joints in total amount to about half of your ability to turn your head. However, the C1-C2 joint alone accounts for the other half. How does that work?
Credit: Illustration by Author
The C1-C2 joint comprises the atlas bone (C1), which rotates around the dens of the axis bone (C2), as shown above. The dens is a tooth-like structure that projects up from C2, which fits into the front of the atlas bone.
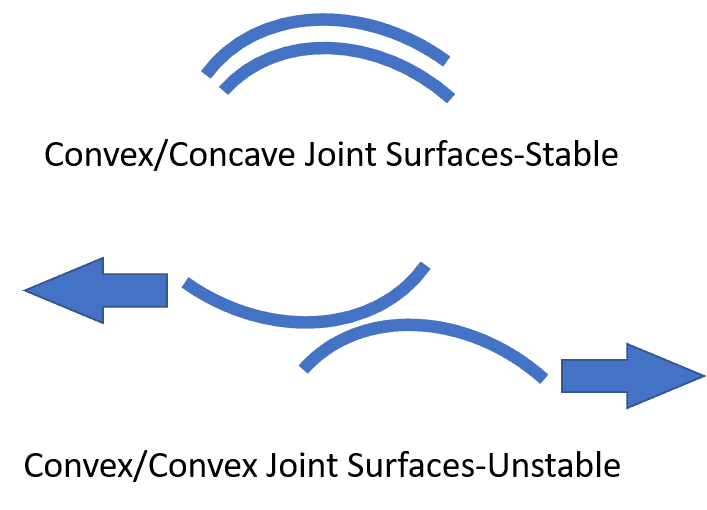
How does this joint accomplish so much rotation when the joints below it each can only rotate a fraction of that amount? Most joints in the body are the ball and socket type. The facet joints from C2-C7 are sliding joints which are how they can allow some rotation of the vertebrae, one on top of the other. The C1-C2 is a very special biconvex joint which is the only one in the body:
Credit: Illustration by Author
This configuration allows an immense amount of rotation of C1 on C2, but it also has an obvious biomechanical problem; it’s inherently unstable. As shown below, this biconvex joint is precarious, with one joint surface being able to fall forward on the other. If that were to happen, that individual would end up with their head and neck stuck to one side, and the cartilage covered joint surfaces would be traumatized:
Credit: Illustration by Author
So how does the body keep the two convex surfaces perched upon each other in that position while C1 rotates around C2?
Meet the Alar Ligament
Credit: Illustration by Author
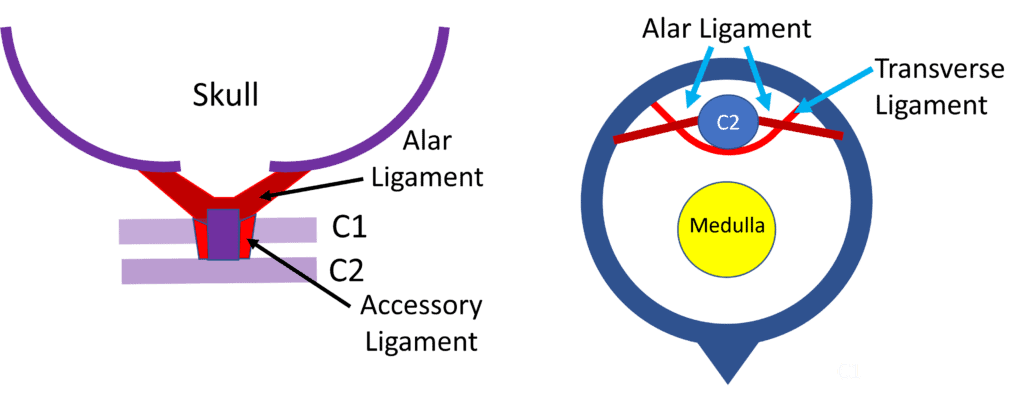
The alar ligament is one of several key structures that bind the skull to the upper cervical spine. The two main ligaments in this area which are considered some of the strongest in the body are the alar and the transverse. The transverse, as shown above, binds the dens of C2 to the atlas and, as such, acts as a “seat belt,” allowing the C1 to rotate safely on C2, as seen above. The alar ligament, in darker red, binds the dens to the skull. As such, it’s in a prime location to prevent lateral motion of C1 on C2 when the patient bends the head to the side. However, it has another role, which is to keep that precarious biconvex joint from getting seriously out of position. Let’s dig in on that concept below.
How the Muscles and Ligaments Work to Stabilize the Spine
So how could the body accomplish the balancing act of keeping one convex joint surface aligned with the other? There are always two sides to the spinal stability equation: muscles and ligaments (4). So let’s back up a bit and first understand how the body stabilizes all parts of the spine.
Muscular stability is how the body stabilizes one vertebra on the other:
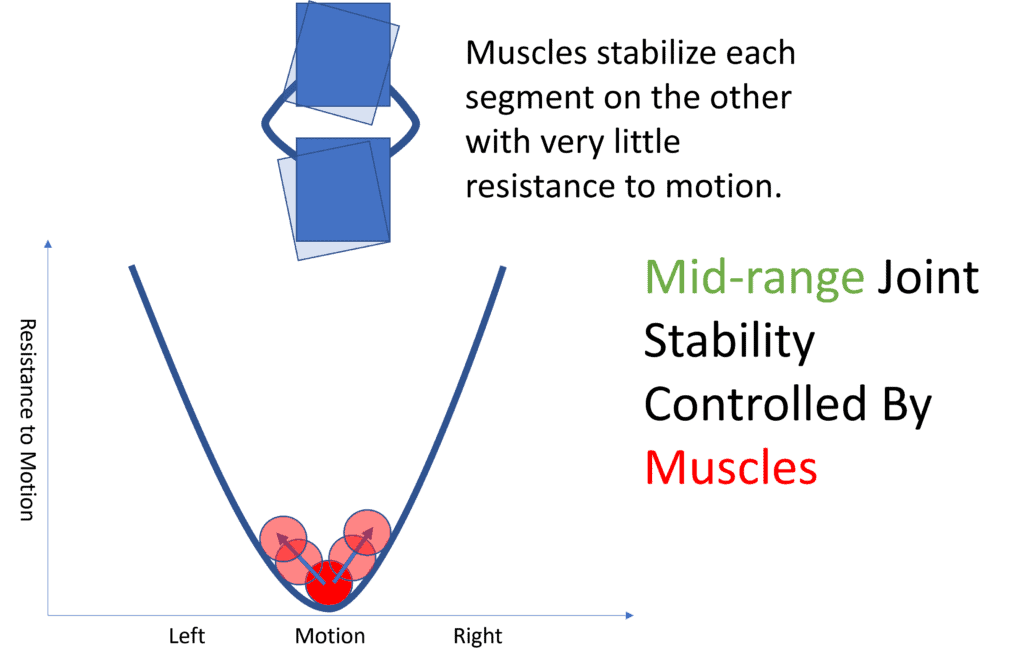
Illustration by Author
Panjabi created the graph above, telling the story of how in the mid-range of spinal movement, the muscles control stability with little resistance to movement. That concept is graphed by considering a ball in a glass, as shown above. The ball always wants to go to the bottom of the glass, which is what a stable spinal segment does as well. In this case, the muscles always tend to bring the spine segment back to its neutral position. In the C1-C2 joint, there are a tremendous number of muscles helping to stabilize that joint:
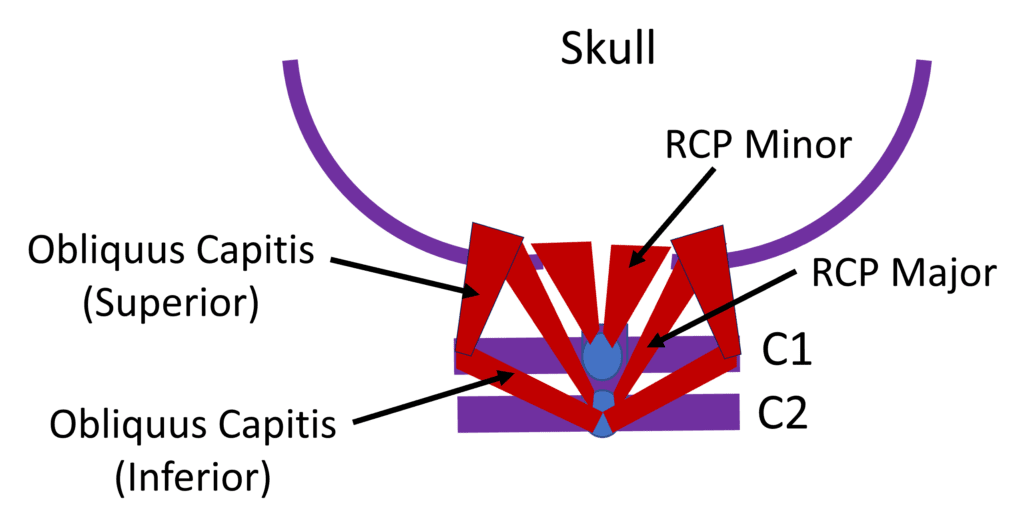
Illustration by Author
However, we also know that patients with traumatically injured necks and headaches have atrophy of these upper cervical stabilizer muscles:
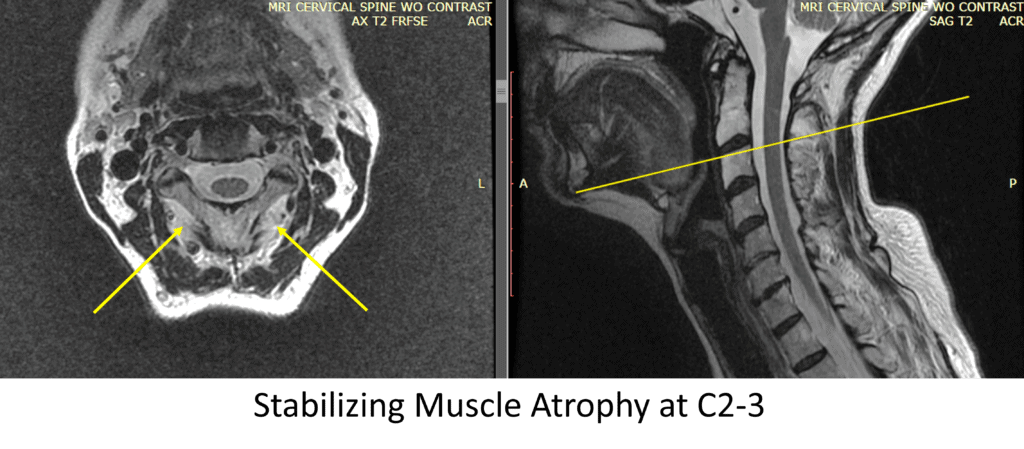
Illustration by the Author
So that means that for patients with traumatic injuries of the upper neck, the stabilizing muscles that provide stability of C1-C2 are atrophied and unable to do their job (5,6). That means that these patients must rely on the ligaments to stabilize that segment:
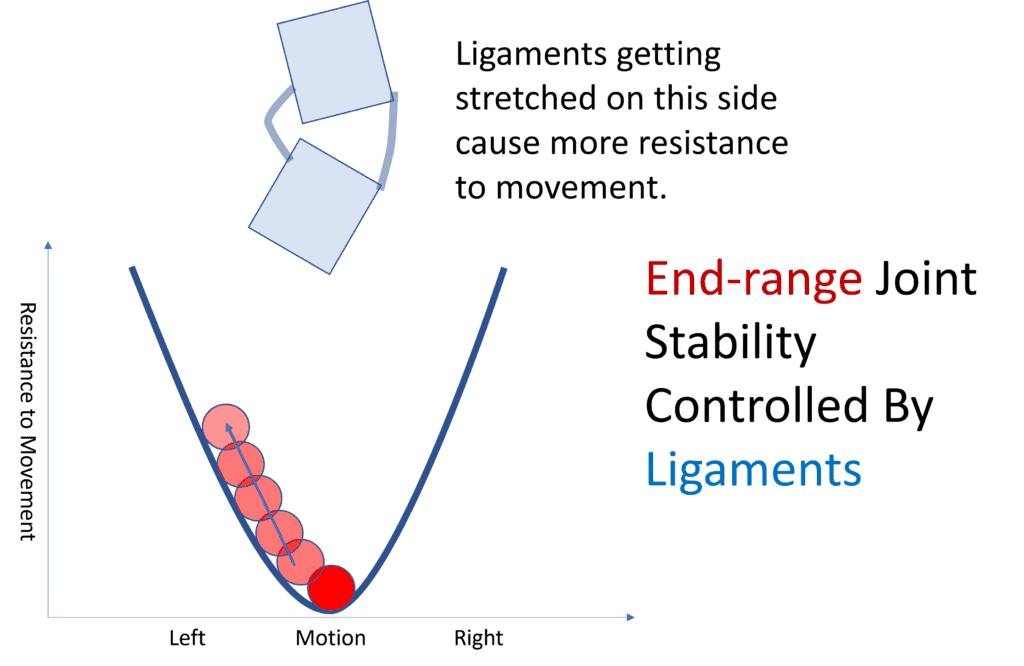
Illustration by Author
In our Panjabi illustration, as the spinal segment moves beyond what the muscles can handle or if the stabilizing muscles aren’t doing their job, the ligaments act as the last defense against the spinal segment dislocating. In this case, we can see the marble going up the wall of the glass with increased resistance to movement, which is what happens when the ligaments engage. You can test this on your finger joint, which will only move so much in extension before the movement stops because of the resistance to motion provided by the ligaments.
How the Alar Ligament Works to Stabilize C1-C2 in Rotation
It’s been known since the 90s and confirmed more recently that in experiments where the alar ligament is cut in cadavers, there is excessive rotation and loss of stability (7, 21). We also know that the C1-C2 capsular ligaments play a role in the overall importance of joint stability within the spine and beyond. However, here, we’ll focus on how the alar ligament helps stabilize C1-C2.
Let’s take the muscles out of the equation and look only at what happens to the alar ligaments when C1 rotates on C2. The ligaments project out from the dens and attach to the skull, so as the skull rotates, they wind around the dens of C2 a bit:
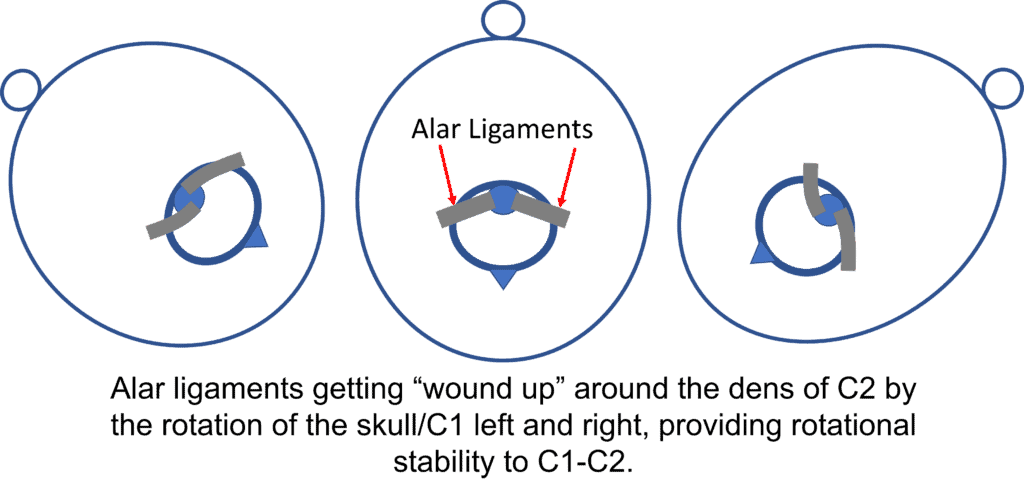
Illustration by Author
What does this look like with an upper cervical model with the alar ligaments?
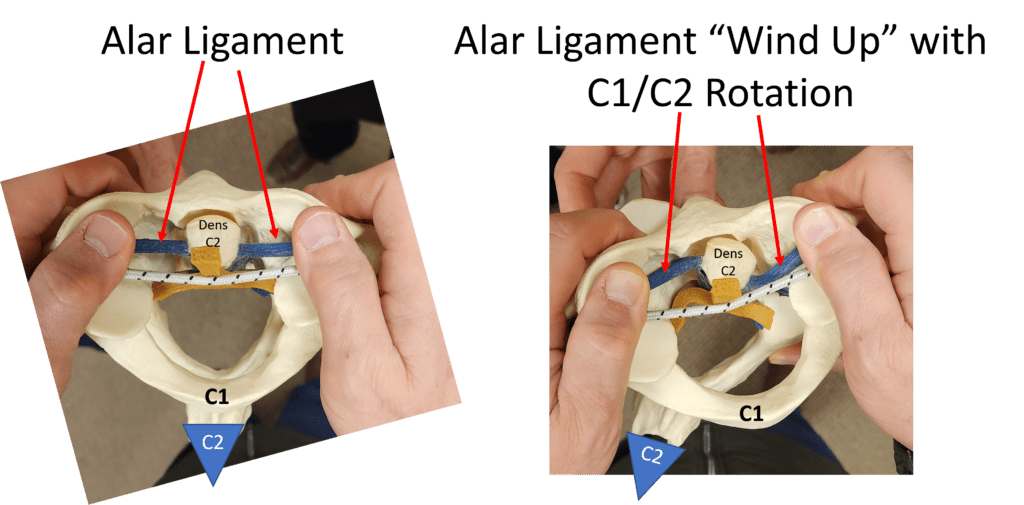
Illustration and photos by the author
Again, notice how the alar ligaments begin to wind around the dens as C1 rotates on C2. So what effect does this have on that precarious C1-C2 biconvex joint?
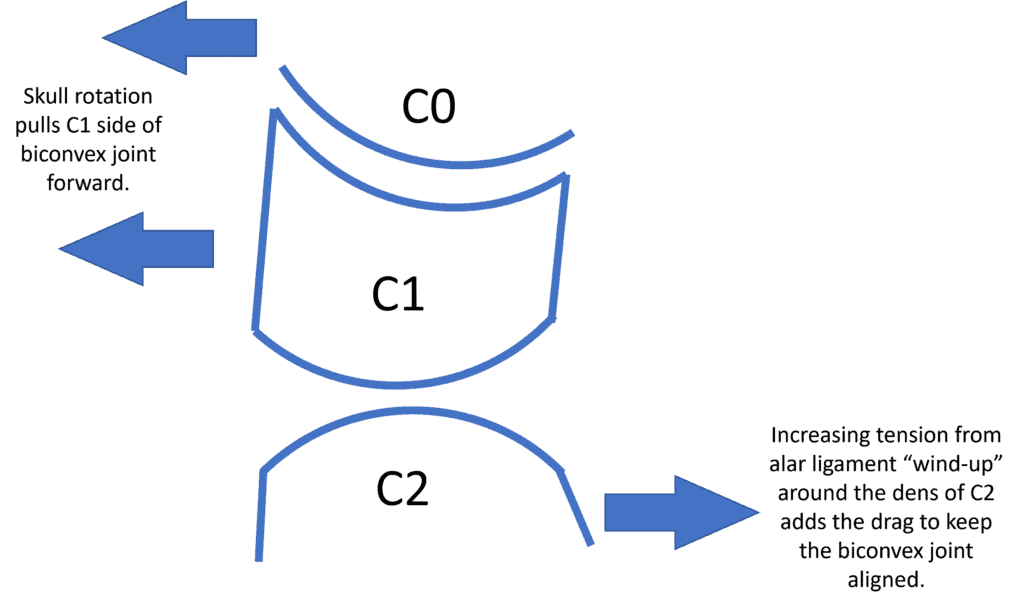
Illustrations by the Author
As C1-C2 rotates, the drag on C2 from those partially wound-up alar ligaments helps the lower part of the biconvex joint to stay aligned with the freely rotating C1 upper part.
Detecting Alar Ligament Laxity
While the alar ligament is strong, like any ligament in the body, it can be injured and become stretched. If so, how would that injury be measured? There are three published methods:
- Rotational CT Scan-Back in the late 80s, before MRIs and movement-based imaging, were a big deal, Dvorak published a paper showing that rotation of C1 on C2 that exceeded 56 degrees was abnormal. (8) This is measured with the head turned maximally to the right and then to the left. The downside is that the population tested here was small, with only nine normal patients and the use of CT Scans markedly increases radiation exposure far above that of x-rays or even videofluoroscopy (9).
- Upper Cervical MRI-Specialized MRI images of the upper cervical spine can show the alar ligaments. Patients with chronic neck pain and headaches have higher signal in those ligaments when compared to normal controls (10,11). These ligaments can be better seen and evaluated on very high field strength 3 T MRI (12). While the original research performed by Krakenes in Norway was on a very specific group of patients chosen by an experienced manual physical therapist as likely to have an upper cervical ligament injury, when this author looked at whether there were signal changes in these ligaments with more commonly injured whiplash patients, there were no differences between injured patients and controls likely due to the low prevalence of traumatic alar ligament injury (13,14). Meaning that this type of cervical MR imaging would only apply to carefully chosen patients and would be a poor screening tool for alar injury.
- Digital Motion X-ray (DMX)-Given that the alar ligament prevents the lateral sliding of C1 on C2, DMX can detect when there is excessive “overhang” of C1 on C2. Katz et al. tested 119 injured and 77 uninjured patients with blinded reviewers measuring various metrics, with 3mm of overhang correctly classifying injured patients 2/3rds of the time and 4mm or more correctly classifying injured patients 95% of the time. Based on this research, in our clinical experience, DMX is the most accurate way to detect an alar ligament injury. (15)
Treating Alar Ligament Laxity
Most of our patients with C1-C2 instability due to alar ligament laxity do very well with upper cervical chiropractic techniques. The goal here is to reposition the atlas on the axis, which in my clinical experience, can result in symptomatic relief. On the other end of the spectrum, C1-C2 fusion is often recommended. However, fusion surgery in this area is generally rife with significant complications (16-20). A middle-ground and less invasive alternative would be the direct injection of the alar ligament with bone marrow concentrate, which the author pioneered, and this treatment is called PICL (Percutaneous Implantation of the Craniocervical Ligaments). In my clinical experience, this procedure has about a 70% success rate in helping patients avoid a fusion. The publication of a large case series is pending.
The upshot? The alar ligament has a unique mechanism for stabilizing C1-C2 in rotation, which is a good thing as this is a precarious joint that is inherently unstable. Laxity in the alar ligament can therefore lead to rotational instability. While C1-C2 fusion is a possible treatment, due to the significant complications of this procedure, direct injection to help the damaged alar ligament heal would make sense as an alternative to fusion.
_________________________________________________________________
References:
(1) Dumas, JL., Sainte Rose, M., Dreyfus, P. et al. Rotation of the cervical spinal column: a computed tomography in vivo study. Surg Radiol Anat 15, 333–339 (1993). https://doi.org/10.1007/BF01627888
(2) Iaccarino C, Francesca O, Piero S, Monica R, Armando R, de Bonis P, Ferdinando A, Trapella G, Mongardi L, Cavallo M, Giuseppe C, Franco S. Grisel’s Syndrome: Non-traumatic Atlantoaxial Rotatory Subluxation-Report of Five Cases and Review of the Literature. Acta Neurochir Suppl. 2019;125:279-288. doi: 10.1007/978-3-319-62515-7_40. PMID: 30610334.
(3) Dreyfuss P, Michaelsen M, Fletcher D. Atlanto- occipital and lateral atlanto- axial joint pain patterns. Spine 1994;19:1125–31.
(4) Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992 Dec;5(4):383-9; discussion 397. doi: 10.1097/00002517-199212000-00001. PMID: 1490034.
(5) Elliott JM, Pedler AR, Jull GA, Van Wyk L, Galloway GG, OʼLeary SP. Differential changes in muscle composition exist in traumatic and nontraumatic neck pain. Spine (Phila Pa 1976). 2014 Jan 1;39(1):39-47. doi: 10.1097/BRS.0000000000000033. PMID: 24270932.
(6) Elliott J, Sterling M, Noteboom JT, Treleaven J, Galloway G, Jull G. The clinical presentation of chronic whiplash and the relationship to findings of MRI fatty infiltrates in the cervical extensor musculature: a preliminary investigation. Eur Spine J. 2009 Sep;18(9):1371-8. doi: 10.1007/s00586-009-1130-6. Epub 2009 Aug 12. PMID: 19672633; PMCID: PMC2899528.
(7) Panjabi M, Dvorak J, Crisco JJ 3rd, Oda T, Wang P, Grob D. Effects of alar ligament transection on upper cervical spine rotation. J Orthop Res. 1991 Jul;9(4):584-93. doi: 10.1002/jor.1100090415. PMID: 2045985.
(8) Dvorak J, Hayek J, Zehnder R. CT-functional diagnostics of the rotatory instability of the upper cervical spine. Part 2. An evaluation on healthy adults and patients with suspected instability. Spine (Phila Pa 1976). 1987 Oct;12(8):726-31. doi: 10.1097/00007632-198710000-00002. PMID: 3686227.
(9) Brenner DJ, Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med. 2007 Nov 29;357(22):2277-84. doi: 10.1056/NEJMra072149. PMID: 18046031.
(10) Chen J, Wang W, Han G, Han X, Li X, Zhan Y. MR investigation in evaluation of chronic whiplash alar ligament injury in elderly patients. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2015 Jan;40(1):67-71. doi: 10.11817/j.issn.1672-7347.2015.01.011. PMID: 25652377.
(11) Krakenes J, Kaale BR, Moen G, Nordli H, Gilhus NE, Rorvik J. MRI assessment of the alar ligaments in the late stage of whiplash injury–a study of structural abnormalities and observer agreement. Neuroradiology. 2002 Jul;44(7):617-24. doi: 10.1007/s00234-002-0799-6. Epub 2002 Jun 8. Erratum in: Neuroradiology. 2002 Oct;44(10):874-6. PMID: 12136365.
(12) Schmidt P, Mayer TE, Drescher R. Delineation of alar ligament morphology: comparison of magnetic resonance imaging at 1.5 and 3 Tesla. Orthopedics. 2012 Nov;35(11):e1635-9. doi: 10.3928/01477447-20121023-22. PMID: 23127456.
(13) Vetti N, Kråkenes J, Damsgaard E, Rørvik J, Gilhus NE, Espeland A. Magnetic resonance imaging of the alar and transverse ligaments in acute whiplash-associated disorders 1 and 2: a cross-sectional controlled study. Spine (Phila Pa 1976). 2011 Mar 15;36(6):E434-40. doi: 10.1097/BRS.0b013e3181da21a9. PMID: 21178847.
(14) Vetti N, Kråkenes J, Ask T, Erdal KA, Torkildsen MD, Rørvik J, Gilhus NE, Espeland A. Follow-up MR imaging of the alar and transverse ligaments after whiplash injury: a prospective controlled study. AJNR Am J Neuroradiol. 2011 Nov-Dec;32(10):1836-41. doi: 10.3174/ajnr.A2636. Epub 2011 Sep 15. PMID: 21920865; PMCID: PMC7965999.
(15) Freeman MD, Katz EA, Rosa SL, Gatterman BG, Strömmer EMF, Leith WM. Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma. Int J Environ Res Public Health. 2020 Mar 5;17(5):1693. doi: 10.3390/ijerph17051693. PMID: 32150926; PMCID: PMC7084423.
(16) Mathers KS1, Schneider M, Timko M. Occult hypermobility of the craniocervical junction: a case report and review. J Orthop Sports Phys Ther. 2011 Jun;41(6):444-57. doi: 10.2519/jospt.2011.3305.
(17) Gluf, W. M., & Brockmeyer, D. L. (2005). Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 67 pediatric patients, Journal of Neurosurgery: Spine, 2(2), 164-169. Retrieved Jan 8, 2020, from https://thejns.org/spine/view/journals/j-neurosurg-spine/2/2/article-p164.xml
(18) Myers KD, Lindley EM, Burger EL, Patel VV. C1-C2 fusion: postoperative C2 nerve impingement-is it a problem?. Evid Based Spine Care J. 2012;3(1):53–56. doi: 10.1055/s-0031-1298601
(19) Schroeder GD, Hsu WK. Vertebral artery injuries in cervical spine surgery. Surg Neurol Int. 2013;4(Suppl 5):S362–S367. Published 2013 Oct 29. doi:10.4103/2152-7806.120777
(20) Ghostine SS, Kaloostian PE, Ordookhanian C, et al. Improving C1-C2 Complex Fusion Rates: An Alternate Approach. Cureus. 2017;9(11):e1887. Published 2017 Nov 29. doi: 10.7759/cureus.1887
(21) Tisherman R, Hartman R, Hariharan K, Vaudreuil N, Sowa G, Schneider M, Timko M, Bell K. Biomechanical contribution of the alar ligaments to upper cervical stability. J Biomech. 2020 Jan 23;99:109508. doi: 10.1016/j.jbiomech.2019.109508. Epub 2019 Nov 23. PMID: 31813563.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
