Interventional Orthopedics: Does It Compete with or Compliment Surgical Orthopedics?
Orthopedic surgery rates are falling ever so slightly due to interventional orthopedics. Will orthopedic surgeons embrace these changes, ignore them, or resist them? Let’s dig in.
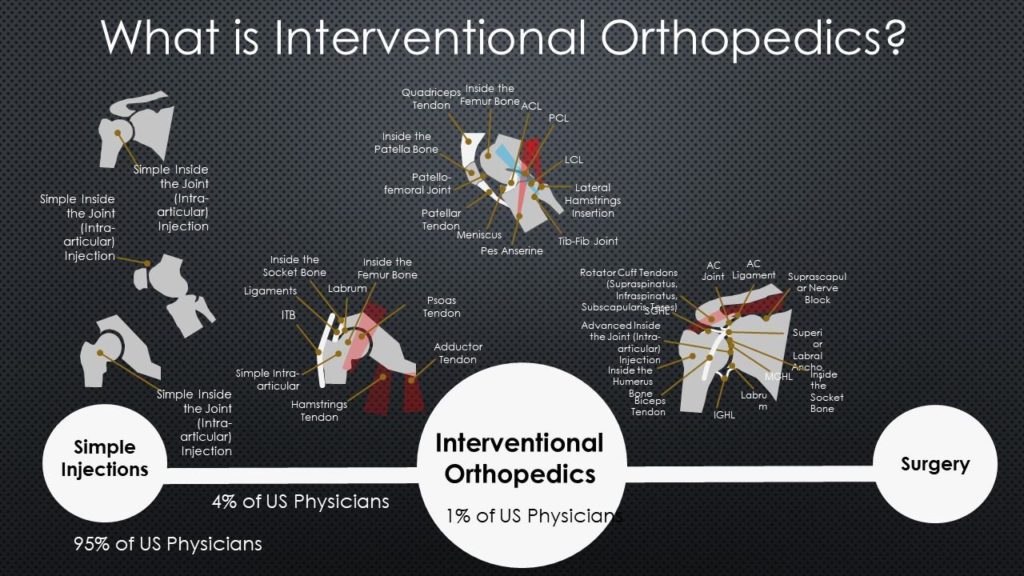
What is Interventional Orthopedics?
The Internet and mobile phones are the fuel for the bonfire of change we have seen in the past two decades. Uber, medical libraries online, Facebook, Amazon, Instagram, all of it dramatically changed the playing field. Orthobiologics are that same change agent in orthopedics.
Right now most orthopedic surgeons fall into two camps on things like stem cells, platelet-rich plasma, or other orthobiologics . One camp gets on its high horse of “we have no proof this stuff works”. A smaller camp knows that there is mounting research showing that orthobiologics work and wants to bolt them onto to traditional surgeries. Then there are the really smart surgeons who are smarter than the other two categories. They see how orthobiologics change the playing field, in the same way that some saw that the Internet and mobile phones would change society long before the first app was created.
Why are orthobiologics that thing that will change how orthopedic care is delivered? Because anything that can be precisely injected using imaging guidance that will help heal damaged orthopedic tissue creates a world where certain surgeries go the way of the dinosaur. For example, take shoulder instability that caused a small labral tear. If the capsular ligaments can be tightened through injection and the labral tear can be healed or helped the same way, surgery just became the more invasive and more expensive way to fix this problem. In addition, the recovery time is cut for the patient as well as the cost, because this injection can be done in the office, pulling cases out of the hospital or ambulatory surgery center.
Interventional orthopedics goes well beyond injecting shoulders, so take a look at my video below:
Orthopedic Surgery Rates Will Fall Dramatically
Based on the discussions of our practice manager with executives who work for local orthopedic surgeons, we know that local surgery rates are dropping. Right now this is just the first ripple of a very big wave. Let me explain.
Let’s take a look at ACL tears. We began using c-arm fluoroscopy to inject these tears with stem cell rich bone marrow concentrate 7-years ago in 2012. In that time we’ve treated 100-200 ACL surgical candidates at our Colorado HQ with Perc-ACLR and turned away about 1 in 3 of them because they had large retracted tears. To understand what Perc-ACLR looks like, check out my video below:
We have seen many of these torn ACL’s heal on post-injection MRI images (1,2). We’ve looked extensively at the failure and complications rates of Perc-ACLR versus Surgical-ACLR. Even when overestimating the costs on the Prec-ACLR side of the ledger, the procedure saves 66% over surgery. The recovery time is about half of ACL surgery and the complication rate is minuscule compared to the more invasive procedure.
So how long will surgical ACLR last in a world where an injection-based procedure is 2/3rd’s cheaper with half the recovery time and a fraction of the morbidity? The first barrier to Perc-ACLR adoption is insurance coverage, but convincing employers who are getting killed by exploding healthcare costs to sign up for a procedure that costs much less is happening. In fact, 7-8 million Americans already have full coverage for Perc-ACLR through Regenexx. So will S-ACLR last another 10 years? Maybe. I doubt that for 2/3rds of the patients who currently get S-ACL that it will last 20 years. Given that there are 100,000 ACL surgeries a year in the US, that’s more than 67K fewer surgeries by 2030 and that’s just one IO procedure out of dozens and dozens which will go head to head with more invasive and expensive surgeries.
Won’t We Have Orthobiologics Plus Surgery?
The short answer is yes, there will always be things that require surgery where an injection won’t work. However, there will also be procedures that can be easily replaced. Those surgeries will die out.
How about surgery plus orthobiologics? That will happen only when the outcomes of orthobiologics plus surgery far exceed interventional orthopedics. I suspect there will be some wins for surgeons here, but their problem will always be that the infrastructure that supports surgery (hospitals, equipment manufacturers, the biologic itself) will always be considered far more expensive than interventional orthopedics performed in a physician’s office. Hence, the outcomes will have to be spectacularly better for surgery for the surgical option to survive.
Winners and Losers
If you’ve been paying attention over the past 20 years, there have been big winners and losers. For example, there used to be something called a travel agent who would book airline tickets. While a few remain, most have disappeared. The same will happen in orthopedics.
If we add 67 K Perc-ACLR procedures to replace S-ACLR procedures, the problem right now is that we only have a few dozen physicians in the US who have any idea of how to properly perform the Perc-ACLR procedure. Hence, we need to train a small army of doctors on how to perform highly complex IO procedures. The Interventional Orthopedics Foundation was created to do just that.
Surgeon Reactions
As I said above, some surgeons are very smart and see this coming. They have already added advanced interventional orthopedics to their practices. However, right now, these surgeons are few and far between. Many have gone the other direction, getting angry that anyone would question their supremacy on the orthopedic care pecking order. I’m sure that’s how the guys who owned Taxi medallions in NYC took it when the first UBER drivers showed up. We all know how that went down.
At Regenexx we have begun to add orthopedic surgeons to our network. These visionaries see where this is heading and are getting ahead of the curve. As surgical rates decline, their bets will be hedged by the members of their groups with IO skills. By being part of the Regenexx network, they also get access to exclusive insurance contracts for coverage of IO procedures. So as revenues decline on one end of the practice, they are buoyed by increases on the other side.
The upshot? I’ll be retired long before many of these changes take hold. By 2040 I’ll be an old man in my seventies, so it’s up to the next generation of physicians to see that as these changes in medicine happen, what’s best for patients gets put first.
_______________________________________________________
References:
(6) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437–447. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4527573/
(7) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6122476/

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
