Introducing “Long-tail” Medicine…
We have always prided ourselves in being a different kind of medical clinic. Our goal has always been to find safe ways to speed new biotechnology to our patients by using our advanced lab facilities, clinical research staff, and bio engineering expertise to reinvent orthopedic care from the ground up. That last statement is an important one, as there’s a push in medicine for the innovation to only occur in the opposite direction – top down. Top down innovation was common in the world of the 1960’s, which birthed our modern regulatory regime. However, like it or not, our world has moved toward what’s been called “The Long-tail”, or long-tail medicine. Over the next few days, I’d like to explore this further. In particular, how this switch from “top down” to “bottom up” innovation will improve medicine. This is also a sneak peak of a larger book I’m writing on medical innovation and the barriers we’re placing in the way:
You take for granted that everything about your life these days has been customized to you. The news that you read has been picked by your friends, or served up based on certain keywords. The stuff advertised on the web page you’re reading is being shown to you based on what you’ve searched for or browsed. The supplements you buy have grown from a few choices with alphabet letters like A, B, and C to a large list of instantly available and endless choice with odd names that are barely recognizable. At the same time that everything is being tailored to what works for you, much of the drugs you take are still being served up like a 1960’s TV dinner – prepackaged and one size fits all. Why?
Our current Food Drug and Cosmetic Act structure was created in 1962, with slight modifications and updates since that time. The world of 1962 had a mass distribution model for everything, including drugs. Distributing anything in the 1960’s was incredibly expensive, so everything from widgets, to new songs, to TV news to drugs had to be distributed in a homogenized way by the millions to be commercially successful. Take a hit song. The cost of promoting the song to record stations, pressing records, and distributing these to stores was massive, so your single better be appropriate for a mass market or you would quickly go bankrupt. That same system today is dramatically different. The single is saved digitally on a computer server with advertising and distribution costs of almost zero – hence the song can appeal to ever smaller niche markets and be commercially successful. Regrettably, even though the stem cell revolution in modern medicine will allow for 21st century niche therapies and true customized medicine, our regulatory system is a 1960’s era model meant to control the mass distribution of homogenized drugs.
What we didn’t know in the 1960s was that all patients are quite different, so mass market drugs made sense to treat what we thought were identical patients. We now know this isn’t even remotely true. Over the next two decades, medicine will undertake a 21st century revamp equivalent to the discovery of modern antibiotics. Although unlike the last big revolution in health care which was focused on “one size fits all” solutions, this one will be focused on individual solutions for unique patients. The problem is that our current 1960’s era mass manufacture regulatory regime will kill much of this innovation. More sinister is that you won’t know about all of the medical miracles you could have had, as without being able to jump through the hoops of this expensive and arcane system, the FDA has literally made it illegal for you to be told about these therapies. In particular, without a regulatory update bringing the FDA’s approach into the 21st century, personalized stem cell therapies, gene therapies, and customized drugs will all be commercial failures, crushed by the gargantuan costs of an antiquated regulatory system.
Take the promise of genetic testing to reduce drug reactions, called pharmacogenetics. Like the flying cars that populated the future of our youth, widespread use of customized medication regimens for patients has only taken hold in a few fields where life threatening disease is common – mainly oncology. Why? Oncology drugs have always been priced much, much higher and many times have lower costs of FDA approval, as the number of patients being treated with any given drug is smaller than the market for a blockbuster drug that everyone takes. These higher prices have allowed some customization of a cancer drug regimen for the individual patient. However, with the high cost of drug approval for most drugs for widespread use, there’s simply no financial incentive for a drug manufacturer to reduce the size of its market by sponsoring research that shows that its drug isn’t effective for patients with a certain genetic makeup. In addition, the reverse is also true. One of the holy grails of pharmacogenetics is the idea that certain drugs that don’t work for the general population may work well in a small subset of patients with unique genetics. Again, with the fully loaded cost of a drug approval at billions of dollars, only drugs that have massive markets get developed. These smaller, custom niche markets will never bear this overwhelming regulatory burden.
What’s the likelihood that we’ll get FDA reform that will allow these individualized therapies to prosper? The issue is that there are big stakeholders in the “one size fits all” frequentist research approach who stand to lose billions if meaningful regulatory reform were to take hold. It’s unlikely that the future of medicine will evolve as it should without another pathway available to doctors, patients, and universities.
In summary, in order for you to truly experience the future of modern medicine, we need another or parallel system that balances access to new therapies, cost, and safety. We need a system that mirrors our current long-tail information age. We need long-tail medicine.
What’s the “Long-tail”?
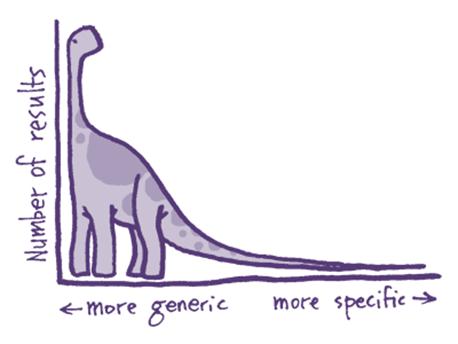
The long tail has revolutionized all aspects of your life. The concept was first described by futurist Chris Anderson to describe how he saw the internet changing our lives and businesses. The basic concept is that information technology allows the business world to sell less of more – meaning that customized content delivered to many people will trump mass market solutions. Since then, most of what you interact with today on the internet follows this strategy. In fact, the only part of society that hasn’t fully embraced this phenomenon is drug development and medicine.
Is long-tail theory applied in medicine at all?
The long-tail is being applied in medicine, but the same kind of fundamental change that we have seen in the rest of society can’t happen because a 1960’s regulatory system is blocking full implementation. Instead, we see bits of pieces of it in information retrieval and in how patients now locate doctors.
As an example, when I was in medical school, researching a single medical subject was an arduous task that performed in any quantity, required armies of librarians. In that time, you went to a medical school library and found one of several massive books known as “Index Medicus”. You then had to be a medical librarian to know which “MESH” subheading encompassed your research interest. You then looked in the Index for the articles that were under that heading. You would invariably miss the newest ones, as the book was out of date the moment it was printed. You then went to the “stacks” and found your medical journal, pulled the publication, took it to the copier, copied your article, and started over for the next subject. I now sit at my computer, with instant access to the US National Library of Medicine, type in my interest, and all relevant articles are delivered in seconds. What used to take weeks can be accomplished in minutes. In fact, this single automated search providing instant access to the world’s most up to date research, has led to more innovation by physicians, who can become instant experts in arcane topics.
Sick patients are also benefitting from the long-tail. A doctor who is very good and learned about treating a little known or studied illness used to have no way to inform the world of his expertise. Now a simple physician website and an internet search engine can connect a patient with an illness and a doctor with expertise, even if the two are a world apart.
While these two small changes have occurred in medicine, most of medical care hasn’t benefitted from the information age because of regulatory barriers to innovation. While the United States is the capital of high tech innovation, this barrier to medical innovation is causing us to lose our number one biotechnology ranking. On a recent trip to China I learned that an iPhone costs the average Chinese worker a few months’ salary, yet the Chinese line up in droves to buy new iPhones from the U.S. While we are leading the world in software and hardware innovation,mostcompaniesarereducinginvestmentinbiotechnologyintheUnitedStates. In fact, many companies are going overseas to innovate.
How much have our regulatory policies driven drug companies out of the United States? In 1999, nearly 27 percent of new drugs approved in the U.S. were first tested in foreign countries. By 2008 that number was a staggering 80%. In fact, in that year, the FDA approved 10 new drugs based entirely on data collected outside the US. Based on attending stem cell conferences and discussing these issues with many members of stem cell drug development teams, the new normal for the biotechnology industry is to seek foreign approval first for your “stem cell drug”. Once the drug is established outside the U.S., the goal is then at some point introduce it to the United States after it’s making money elsewhere. Only at that point will some of these companies try to navigate the FDA gauntlet. Practically, this means in many instances that foreign citizens will be accessing the most advanced biotechnology well before U.S. citizens get access to the technology that was funded by their tax dollars!
More to come tomorrow…

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.