Is a Rocky Mountain High a Problem for Your Regen Procedure?

Credit: Shutterstock
I live in the highest state in the Union, both in reality and figuratively. Given that Colorado has had legal recreational marijuana sales for more than a decade, I’ve noticed a few trends with cannabis use and patients undergoing regenerative medicine procedures. Now new national guidelines have concluded that cannabis use is very important for physicians to begin noting as it increases the complexity of managing post-op pain. Let’s dig in.
Rocky Mountain High
Colorado legalized recreational marijuana in 2012. More than 1 in 4 adults here use cannabis. Hence, I’ve had lots of time to form an opinion about how that impacts our regenerative medicine procedures.
One of the things I noticed years ago was that getting a regular cannabis user to sleep using IV anesthesia was just as hard as sedating a high-dose opioid user. Meaning both patients took huge amounts of medications to get to the point where they were unconscious. Obviously, any time you’re using 2-3X the normal dose of anesthetic agents to keep the patient asleep during a procedure, that increases anesthesia risk.
The Good, The Bad, and the Ugly
Given that so many patients are using cannabis and that these percentages are likely even higher among patients in pain, how does this impact these procedures? What does the existing research show about how cannabis use impacts stem cells?
In this research review, I’ll focus on mesenchymal stem cells (MSCs), which are believed to be the active ingredient in both bone marrow concentrate and adipose procedures.
The Good?
Can cannabis use help your stem cells? Years ago, the jury was out on that, and the data pointed to more problems than help. However, has that cleared up and changed? Let’s dive into this research.
Before we review these studies, it’s critical to note that we have no actual clinical data on how cannabis use impacts the outcome of a regen med procedure. The papers we’re reviewing here are all lab or animal models, so this data may or may not apply directly to real patients.
One animal study of skin wound closure that used adipose and bone marrow-derived allogeneic stem cells show faster wound healing in cells pre-treated with CBD and THC (1). Another lab and animal study demonstrated that phytocannabinoids promote the viability of bone marrow mesenchymal stem cells, but they also promoted them to turn into adipose cells (2). This is consistent with earlier research I highlighted years ago showing this same trend, which is not a good thing for an orthobiologic injection where we’re trying to create new cartilage, ligament, or tendon tissue.
When focusing on a cartilage repair application for MSCs, Gowran et al. demonstrated that activating the cannabinoid system helped the survival, migration, and chondrogenic differentiation (cartilage formation or repair) of MSCs (5). Jamshidi et al. observed that Sativa extract did not impact the osteoblastic differentiation potential (bone formation or repair) of adipose-derived MSCs (6).
Dose may play a role in how these compounds impact mesenchymal stem cells. For example, in one study of an extract from Sativa marijuana, lower doses for the short-term helped MSC proliferation, and higher doses and longer exposures killed the cells (3). Similar dose effects have been seen when Delta THC was exposed to neural cell lines (4).
How does all of this work? MSCs contain cannabinoid receptors (CB1 and CB2). Gowran et al. found that when the CB1 receptor on MSCs is activated, it promotes cell survival. However, Delta-THC has a negative impact on MSC survival and bone formation, with the author adding a warning for orthopedic patients that use THC (7). Yan observed that this CB1 receptor on bone-marrow MSCs enhances the bone formation of bone-marrow MSCs when they are exposed to an inflammatory environment (8).
Can we make sense of all of these findings? Studies focusing on exposing MSCs to small amounts of THC or CBD can show positive effects, but the dose and length of exposure probably matter, as this can go in the other direction. Specific elements of the cannabinoids like Delta-THC may have a more negative effect.
The Bad
How does regular THC use impact the anesthesia used in many of these procedures?
Several studies show that cannabis users require more anesthesia medication to stay asleep (10,11). However, the anesthesia only becomes more dangerous when the patient is abusing cannabis (12). On the other side of this debate, one study found no difference in the amount of anesthesia medications between control and cannabis patients (9).
My personal experience here is more consistent with higher doses of anesthesia being needed in patients who use cannabis products regularly. These patients tend to be more of the “tightrope” anesthesia type, very similar to patients on opioids. What’s that? They require more medications and are tough to keep in that place where they are asleep and well-oxygenated. This means that they can easily move into the awake category despite high medication doses, or they are so obtunded by these large doses that they begin to drop their blood oxygenation. Hence, it’s always a challenge to keep them asleep and safe simultaneously, so I educate these patients that they are in a higher-risk anesthesia category.
The Ugly
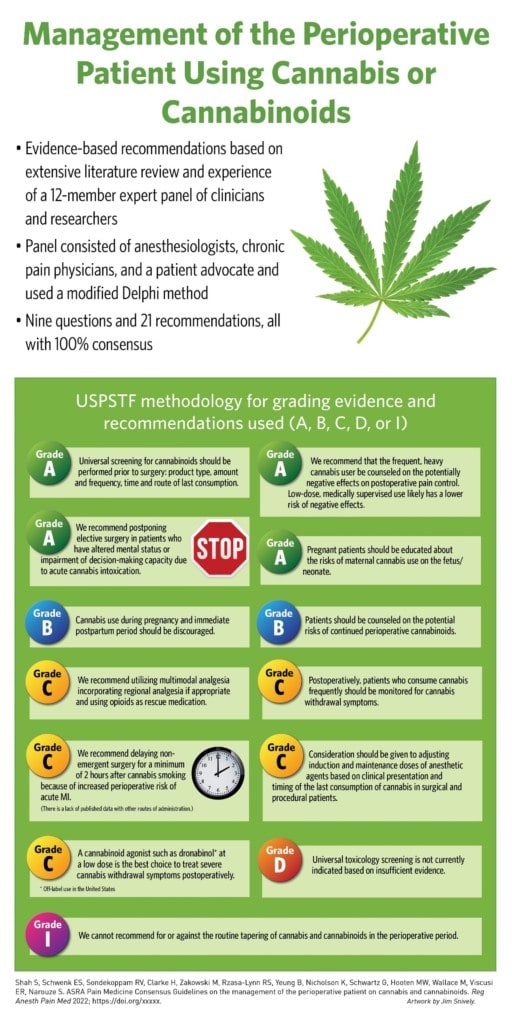
The ASRA Pain organization (focused on regional anesthesia techniques) just posted new evidence-based guidelines on cannabis use and anesthesia (13). One of the more surprising conclusions based on a review of the literature was:
“Chronic use of THC may worsen postoperative pain, increase postoperative opioid use and precipitate the development of postoperative hyperalgesia. Level of certainty: Moderate”
In other words, regular cannabis users tend to have problems managing their post-procedural pain. This is something I frankly hadn’t considered, as I have never tried to connect the dots between a severe procedure pain flare and cannabis use. However, this makes sense, as anesthesia for a regular cannabis user resembles a heavy opioid user, and those patients also have post-procedural pain management challenges.
Here are the rest of the conclusions in infographic form (click to see a bigger version):
My new recommendations:
- If you’re an every day cannabis user, reduce your dose significantly 4-6 weeks before and after your regen med procedure. If you’re a social weekend user, avoid using high doses on the weekends.
- If you’re using cannabis regularly for pain control, realize that this will likely increase your medication requirements and anesthesia risk and may make it harder to control pain after your procedure.
The upshot? Cannabis research is evolving rapidly. I would say the jury is very much still out on if this impacts a regen med procedure as we don’t have actual studies in patients receiving these procedures and comparing outcomes, just lab, and animal research. However, there seems to be an evolving consensus that regular cannabis use plus anesthesia can create issues and that these patients have a harder time managing their pain after a procedure.
______________________________________________
References
(1) Miller H, De Leo N, Badach J, Lin A, Williamson J, Bonawitz S, Ostrovsky O. Role of marijuana components on the regenerative ability of stem cells. Cell Biochem Funct. 2021 Apr;39(3):432-441. doi: 10.1002/cbf.3609. Epub 2020 Dec 21. PMID: 33349985.
(2) Fellous T, De Maio F, Kalkan H, Carannante B, Boccella S, Petrosino S, Maione S, Di Marzo V, Iannotti FA. Phytocannabinoids promote viability and functional adipogenesis of bone marrow-derived mesenchymal stem cells through different molecular targets. Biochem Pharmacol. 2020 May;175:113859. doi: 10.1016/j.bcp.2020.113859. Epub 2020 Feb 14. PMID: 32061773.
(3) Sazmand, Maryam & Mehrabani, Davood & Hosseini, Ebrahim & Amini, Masood. (2018). The effect of hydroalcoholic extract of Cannabis Sativa on morphology and growth of bone marrow mesenchymal stem cells in rat. 15. 10.29333/ejgm/86195.
(4) Chen J, Lee CT, Errico S, Deng X, Cadet JL, Freed WJ. Protective effects of Delta(9)-tetrahydrocannabinol against N-methyl-d-aspartate-induced AF5 cell death. Brain Res Mol Brain Res. 2005;134(2):215-225. doi:10.1016/j.molbrainres.2004.10.044
(5) Gowran A, McKayed K, Kanichai M, White C, Hammadi N, Campbell V. Tissue Engineering of Cartilage; Can Cannabinoids Help?. Pharmaceuticals (Basel). 2010;3(9):2970-2985. Published 2010 Sep 6. doi:10.3390/ph3092970
(6) Jamshidi M, Hosseini S E, Mehrabani D, Amini M. Effect of hydroalcoholic extract of Cannabis sativa on cell survival and differentiation of mesenchymal stem cells derived from human adipose tissue to osteoblast-like cells. J Gorgan Univ Med Sci 2019; 21 (2) :50-58
(7) Gowran A, McKayed K, Campbell VA. The cannabinoid receptor type 1 is essential for mesenchymal stem cell survival and differentiation: implications for bone health. Stem Cells Int. 2013;2013:796715. doi:10.1155/2013/796715
(8) Yan W, Li L, Ge L, Zhang F, Fan Z, Hu L. The cannabinoid receptor I (CB1) enhanced the osteogenic differentiation of BMSCs by rescue impaired mitochondrial metabolism function under inflammatory condition. Stem Cell Res Ther. 2022 Jan 21;13(1):22. doi: 10.1186/s13287-022-02702-9. PMID: 35063024; PMCID: PMC8781353.
(9) King DD, Stewart SA, Collins-Yoder A, Fleckner T, Price LL. Anesthesia for Patients Who Self-Report Cannabis (Marijuana) Use Before Esophagogastroduodenoscopy: A Retrospective Review. AANA J. 2021;89(3):205-212.
(10) Kraft B, Stromer W. Der Einfluss von Cannabis und Cannabinoiden auf Anästhesie und Analgesie in der perioperativen Phase [The effects of cannabis and cannabinoids on anesthesia and analgesia during the perioperative period]. Schmerz. 2020 Aug;34(4):314-318. German. doi: 10.1007/s00482-020-00449-x. PMID: 32125500.
(11) Lynn RSR, Galinkin JL. Cannabis, e-cigarettes and anesthesia. Curr Opin Anaesthesiol. 2020 Jun;33(3):318-326. doi: 10.1097/ACO.0000000000000872. PMID: 32371642.
(12) Goel A, McGuinness B, Jivraj NK, Wijeysundera DN, Mittleman MA, Bateman BT, Clarke H, Kotra LP, Ladha KS. Cannabis Use Disorder and Perioperative Outcomes in Major Elective Surgeries: A Retrospective Cohort Analysis. Anesthesiology. 2020 Apr;132(4):625-635. doi: 10.1097/ALN.0000000000003067. PMID: 31789638.
(13) Shah S, Schwenk ES, Sondekoppam RV, et alASRA pain medicine consensus guidelines on the management of the perioperative patient on cannabis and cannabinoidsRegional Anesthesia & Pain Medicine Published Online First: 03 January 2023. doi: 10.1136/rapm-2022-104013

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.