Understanding Scoliosis: A Guide To Spinal Curvature

Medically Reviewed By:
Scoliosis affects millions, presenting unique challenges that may impact posture, mobility, and daily life. While commonly identified in childhood, it can emerge at any age, with varying severity and symptoms. Understanding scoliosis—its causes, signs, and available treatments—may be important for managing the condition.
This article provides an in-depth look at scoliosis, helping you recognize symptoms and explore options that may help support a healthier spine and overall well-being.
Defining Scoliosis
Scoliosis involves an abnormal spine curvature that may place uneven pressure on different spinal regions, increasing the risk of further misalignment over time. Imagine a stack of blocks: if one block shifts out of place, the entire stack loses stability.
Similarly, a curved spine can disrupt the balance and alignment of surrounding muscles and tissues, complicating efforts to maintain proper posture and movement. Gravity continuously acts on this misalignment, and in some cases, this may contribute to the progression of curvature, potentially leading to discomfort or mobility limitations.
The severity of scoliosis varies widely, ranging from minor curves that cause no symptoms to significant bends that interfere with daily activities. While a healthy spine’s natural curve distributes weight evenly, scoliosis may alter this distribution. Understanding scoliosis’s different types and causes may be important for determining the best management approach.
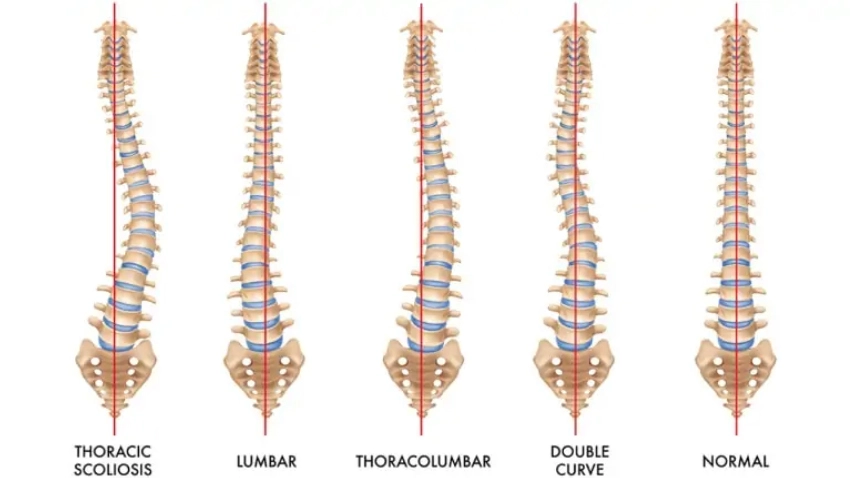
Below is a medical illustration showing a healthy spine alongside others affected by different forms of scoliosis. This highlights the range of possible curvatures and how each type may alter spinal alignment.
It is often assumed that an abnormal MRI of the spine directly correlates with pain. However, research has shown that these findings should be interpreted in context, as spinal abnormalities do not always correlate with pain levels. Some individuals with significantly abnormal spinal appearances experience minimal or no pain, while others with relatively normal-looking spines report significant discomfort.
Nevertheless, it is difficult for physicians to overlook these findings when severe scoliosis or stenosis is present due to the potential impact on function and mobility.
Central canal stenosis occurs when the opening in the middle of each vertebra, called the spinal canal, becomes narrowed, often due to the development of bone spurs or thickened ligaments. Because this space houses nerves responsible for leg movement and sensation, stenosis may lead to weakness or numbness, especially when standing, as this position can increase nerve compression more than sitting.
Types Of Scoliosis
Scoliosis can be classified into several types, each with distinct characteristics, causes, and implications for treatment. Identifying the type of scoliosis may be important for determining the most suitable management strategies. Below are the primary types:
- Idiopathic scoliosis: Idiopathic scoliosis is the most common type, especially among adolescents, and it has no identifiable cause. It often develops during growth spurts and may be influenced by genetic factors. Severity can vary, and treatments range from regular observation to more active interventions.
- Congenital scoliosis: Present at birth, congenital scoliosis arises from abnormal vertebral development in the womb. Congenital scoliosis may involve malformed or fused vertebrae, leading to an early and often progressive spinal curve. Treatment typically includes close monitoring, while more severe cases may require surgical intervention to address alignment.
- Neuromuscular scoliosis: Neuromuscular scoliosis develops in individuals with conditions affecting the nerves and muscles, such as muscular dystrophy, cerebral palsy, or spinal cord injury. Weak or imbalanced muscles may exert uneven force on the spine, resulting in curvature. Management may include customized bracing or surgery to help support spinal stability and manage progression.
- Degenerative scoliosis: Primarily affecting adults, degenerative scoliosis results from age-related spinal degeneration. The spine may curve as spinal discs and joints deteriorate, which can cause pain, stiffness, and possible nerve compression. Treatments often focus on physical therapy, pain management, and, in some cases, surgery to address symptoms and help prevent further curvature.
- Traumatic scoliosis: Caused by spinal injury, such as a fracture or dislocation, traumatic scoliosis can develop if the spine heals improperly or if the injury destabilizes it. Treatment typically focuses on stabilizing the spine, with surgical correction considered based on the severity of the injury.
Scoliosis Vs Stenosis
Scoliosis and stenosis are distinct spinal conditions that may share symptoms like back pain and limited mobility. While both conditions can be associated with discomfort, they affect different parts of the spine and may result in varied symptoms.
- Scoliosis: Scoliosis involves a sideways curvature of the spine that may impact posture and balance. This condition can contribute to muscle fatigue, pain, and restricted movement. As scoliosis progresses, the curvature may pressure nerves, leading to discomfort and, in some cases, additional mobility limitations.
- Stenosis: Stenosis occurs when the spinal canal narrows, compressing both the spinal cord and nerves, which may result in symptoms like pain, tingling, and numbness. Unlike scoliosis, which primarily involves structural curvature, stenosis commonly develops with age and may be linked to spinal disc and joint degeneration. Stenosis can restrict the space within the spinal canal, potentially leading to nerve irritation.
Key Causes And Risk Factors
Understanding the causes and risk factors of scoliosis may help identify individuals at higher risk for developing the condition and support early detection efforts. Although scoliosis can occur at any age, several factors may contribute to its onset and progression. Below are key causes and risk factors that may be associated with scoliosis.
- Family History of Spine-Related Conditions: A family history of scoliosis or other spine issues may be linked to an increased likelihood of developing scoliosis, as genetics could play a role.
- Vertebral Malformation During Fetal Development: Abnormal spinal development in the womb, such as fused or malformed vertebrae, may lead to congenital scoliosis.
- Poor Posture: While not a direct cause, prolonged poor posture may contribute to muscle imbalances and spinal strain, which could impact spinal alignment over time.
- Leg Length Discrepancy: Differences in leg length can affect alignment and posture, placing uneven pressure on the spine and potentially influencing scoliosis progression.
- Neuromuscular Disorders: Conditions affecting nerves and muscles, such as cerebral palsy or muscular dystrophy, may contribute to scoliosis due to uneven muscle support around the spine.
- Spinal Injuries or Infections: Trauma or infection in the spine can result in structural changes, leading to curvature or instability that could contribute to scoliosis.
- Spinal Cord Abnormalities: Conditions like tethered cord syndrome may affect spinal development and alignment, which could increase scoliosis risk.
Common Symptoms Of Scoliosis
Scoliosis can cause various symptoms affecting posture, movement, and comfort. Recognizing these signs early may help support condition management. Common symptoms may include:
- Visible Spinal Curve: A noticeable curve in the spine, often more apparent when bending forward.
- Uneven Shoulders, Hips, And Waist: One shoulder, hip, or side of the waist may appear higher.
- Prominent Shoulder Blade: One shoulder blade may protrude more than the other.
- Body Leaning To One Side: The body may appear to tilt or lean due to the spinal curvature.
- Difficulty Breathing: In severe cases, the spinal curve may pressure the lungs, making breathing more difficult.
- Fatigue: Muscle strain from compensating for the spinal curve may contribute to fatigue, especially after prolonged standing or activity.
Diagnostic Methods To Detect Scoliosis Early
Early detection of scoliosis may be important for effective management and could help reduce the likelihood of the curvature progressing further. Diagnosis usually involves the following:
- Physical examination: A healthcare provider may assess signs of scoliosis, such as uneven shoulders or hips, during a routine physical exam. A standard screening method is the Adam’s Forward Bend Test, in which the patient bends forward to reveal any spinal asymmetry.
- X-rays: X-rays are often used to confirm the diagnosis and evaluate the severity of the curve. They provide a detailed view of the spine’s alignment and help measure the degree of curvature, which may be important for treatment planning.
- MRI or CT scans: If additional detail is needed, particularly when symptoms of nerve compression are present, a physician may recommend an MRI or CT scan. These scans provide a clearer view of the spinal cord and any potential stenosis, allowing for a comprehensive assessment.
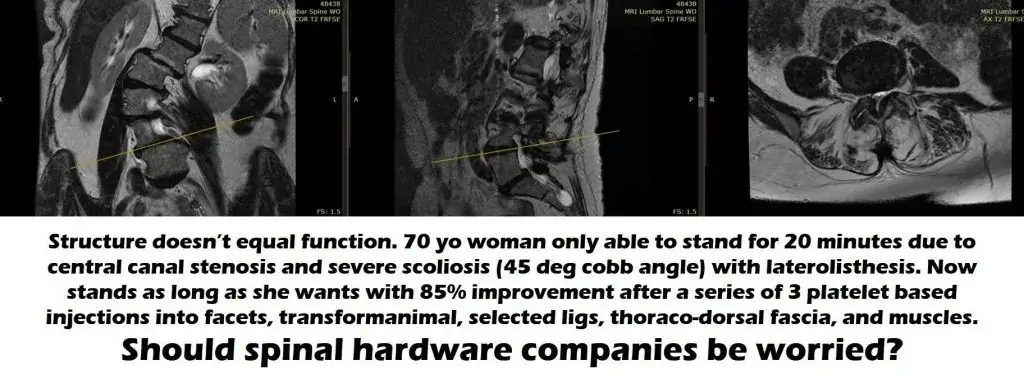
Looking at the MRI image on the left, it is evident that the spine typically appears straight when viewed from the front. However, this spine displays an “S” shape, which suggests that one vertebra may have shifted to the right, indicating misalignment.
Severe stenosis is visible in the image to the far right, which may suggest a surgical need. However, non-surgical options may also be available to address these complex conditions.
Non-Surgical Scoliosis Care With Regenexx
For individuals seeking alternatives to surgery, non-surgical treatments may help manage scoliosis symptoms and promote a better quality of life. Procedures using Regenexx injectates, along with targeted therapies, can help reduce pain and improve function. Below is an overview of available non-surgical care options:
- Physical therapy: Customized exercises focus on strengthening the muscles surrounding the spine, supporting posture, and relieving tension caused by the spinal curve.
Recognizing The Right Time To Seek Treatment For Scoliosis
Recognizing when to seek treatment for scoliosis may play a role in managing the condition. The following signs may indicate it is time to consult a healthcare provider:
- Noticeable curve in the spine: A visible spine curve, especially when bending forward, may signal the need for a professional evaluation.
- Persistent pain: Mild discomfort is common, but persistent back or neck pain that disrupts daily activities may warrant medical attention.
- Increasing asymmetry: Uneven shoulders, hips, or a prominent shoulder blade may suggest scoliosis progression and should be assessed.
- Changes in posture or mobility: A noticeable shift in body alignment or challenges with balance may indicate that an evaluation could be beneficial.
- Breathing difficulties: In severe cases, scoliosis may impact lung function. Experiencing shortness of breath during routine activities may be a reason to seek care.
- Fatigue during standing or walking: Muscle strain around the spine that leads to fatigue, especially when walking or standing, may indicate the need for intervention.
Identifying these signs early and consulting with a physician or specialist may help support effective management strategies to help reduce the risk of further complications and promote comfort and mobility.
Scoliosis Can Be Managed: Explore Your Care Options
Living with scoliosis does not have to mean facing limitations. With the right care and a proactive approach, scoliosis management may help maintain mobility, address discomfort, and support overall function. Treatment options customized to your unique needs—such as physical therapy, lifestyle modifications, or specialized non-surgical approaches—may help support long-term spine health and well-being.
Connect with a physician in the licensed Regenexx network to explore your non-surgical care options.
To talk one-on-one with one of our team members about how Regenexx may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
