Is Surgery Necessary for a Torn Meniscus? More Research
Is surgery necessary for a torn meniscus? The answer, based on the research, is now clear. If you’re over age 35, the most common surgery used to treat a torn meniscus called partial meniscectomy is useless. Now new research out of Johns Hopkins quantifies the massive scale of the epidemic of ineffective knee meniscus surgeries . Let’s dig in.
What Is a Meniscus?
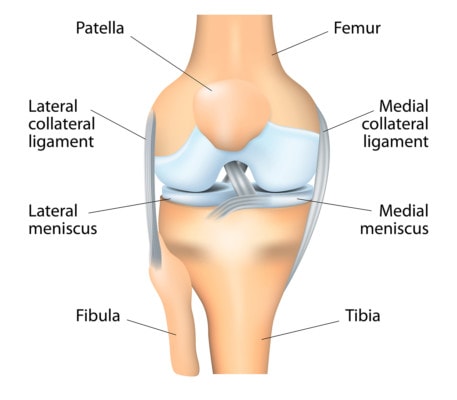
Anatomy of the knee. Designua/Shutterstock
The meniscus in the knee is a piece of tissue that’s shaped like a figure 8. The two rounded ends of the thigh bone sit in each one of the circles of the figure 8. The meniscus is a spacer that keeps the bones apart and also supplies some stability for the joint.
The meniscus can tear. There are many different types and locations of tears, which may or may not have some significance as it relates to recovery. Research has shown that meniscus tears as we age are very common and should be treated with the same concern as wrinkles. (1)
Does a Torn Meniscus Cause Pain?
The first question anyone who has a meniscus tear on MRI asks themselves is, “Is surgery necessary for a torn meniscus? Before answering that question, we need to answer a simpler one. Is the torn meniscus causing your knee pain?
If you just got your MRI CD or link to the patient portal online, you may want to watch my video on how to read those images:
Regrettably, we as physicians, have educated several generations of patients to get alarmed when they see a meniscus tear on an MRI report. The idea was supposed to be that there was a strong correlation between a meniscus tear and pain. However, many research studies have debunked this idea. Patients with and without knee pain both have meniscus tears with about the same frequency (2).
In summary, in middle-aged patients, finding a meniscus tear on an MRI in a patient with knee pain should, for the most part, be ignored. This is because there is unlikely to be a connection between that tear and why your knee hurts. Hence, planning surgery on a structure that isn’t causing the pain in the first place may be a bad idea. However, we’ll explore that next.
Is Surgery Necessary for a Torn Meniscus?
The most common surgery for a torn meniscus is called an arthroscopic partial meniscectomy (APM). This means that the surgeon removes the torn part. Only a handful of meniscus surgeries are meniscal repairs, despite patients often believing that their surgery will “repair” their meniscus tear (3). Hence, if you have been told you need knee surgery to treat a meniscus tear, there’s a greater than 90% chance it’s an APM surgery.
There have been many high-quality research studies over the past decade or more that were designed to answer the specific question, “Is surgery necessary for a torn meniscus?”. What did they show? No matter what the clinical scenario: meniscus tear with arthritis, meniscus tear without arthritis, or locking of the knee, all three large studies showed that meniscus surgery was not effective or no better than just physical therapy (4,5,6).
New Research from Johns Hopkins
This new research first recognized that based on the published research we reviewed above showing that meniscectomy is ineffective, orthopedic surgeons should be phasing out the procedure (7). To learn more they reviewed hundreds of thousands of knee surgeries. What did they find? Two-thirds of all arthroscopic knee surgeries are still partial meniscectomies! The authors concluded:
“These data suggest a significant and troubling disparity between evidence and practice for one of the most common operations performed in the United States.”
Hence, we have a huge disparity between the research that tells us orthopedic surgeons should no longer be offering these procedures, and, actual practice where they are still commonly offered. Why? I suspect that if the average US hospital or university medical center were to get rid of 2/3rds of its knee surgery cases by phasing out meniscectomy, it wouldn’t be able to make payroll.
Can Menisectomy Be Harmful?
All surgeries have risks. Meniscectomy is no different and those risks include infection, blood clots, nerve damage, etc… However, most patients don’t know or are never told that there is research suggesting that meniscectomy may increase the likelihood for arthritis (8). In one study, the authors found that patients who had meniscectomy were 4.5 times as likely to develop arthritis versus those patients who didn’t have the surgery.
Is There a Better Way?
We’ve been treating patients with knee meniscus tears with precise ultrasound and x-ray guided injections of orthobiologics for many years, see my video below for more information:
In addition, I have written a whole book on ways to avoid knee surgery:
The upshot? Despite all of the research showing that meniscectomy should be a procedure that physicians retired years ago, it’s still the most common knee surgery in the United States. Hence, don’t let yourself be a knee surgery victim, do your homework!
References:

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.