Is There Objective Evidence that PRP Helps Tendons Heal? Concentration and Age Matter
This has been an interesting few months in the world of PRP research. We’ve seen a few studies that purport to show that PRP doesn’t work, after dozens of similar studies that showed it was effective. While it turns out that the studies that seemed to show that PRP was ineffective never used actual PRP or underdosed it, what about studies that use objective evidence to show that higher-dose PRP helps damaged tendons heal? Let’s dig in.
A Recent Fake PRP Tendon Study
I have already blogged on a poorly done study published in 2021 where PRP was injected into patients with Achilles tendinopathy (1). The study presumed to show that PRP didn’t work for this application, but there were significant issues. First, the PRP was very underdosed based on age. Meaning a 3-4X PRP was used in patients with a mean age of 52 which based on our research on how tenocytes respond to PRP was about 1/3 to 1/2 of the dose needed to get the best healing response (2). The other was that the injections were blind, which is below the standard of care in 2022, as some percentage of them likely missed the tendon altogether or injected into the sheath rather than the substance of the tendon itself.
PRP Dosing 101
PRP means platelet-rich plasma. The doctor takes whole blood from a vein and concentrates the platelets in the plasma. In order for the end product to be considered PRP, the mix has to have at least 2X or twice the platelets of the original blood. Hence a 3X PRP has three times and a 10X has ten times more platelets than the original blood.
A More Recent Real PRP Tendon Study
A new study was just published that treated patients with tennis elbow (lateral epicondylitis) who were on average 54 years of age (3). However, they also used PRP which was more concentrated at 5X, which is still low for this age group, but better. A similar blind technique was used, but in this study the target is much easier to hit blind, meaning that you’re more likely to be injecting into the tendon itself than around the tendon when compared to the study above. 30 patients were treated with a single PRP injection and then serial 3T MRIs were performed at 1, 3, 6, 12, 18, and 24-month follow-ups.
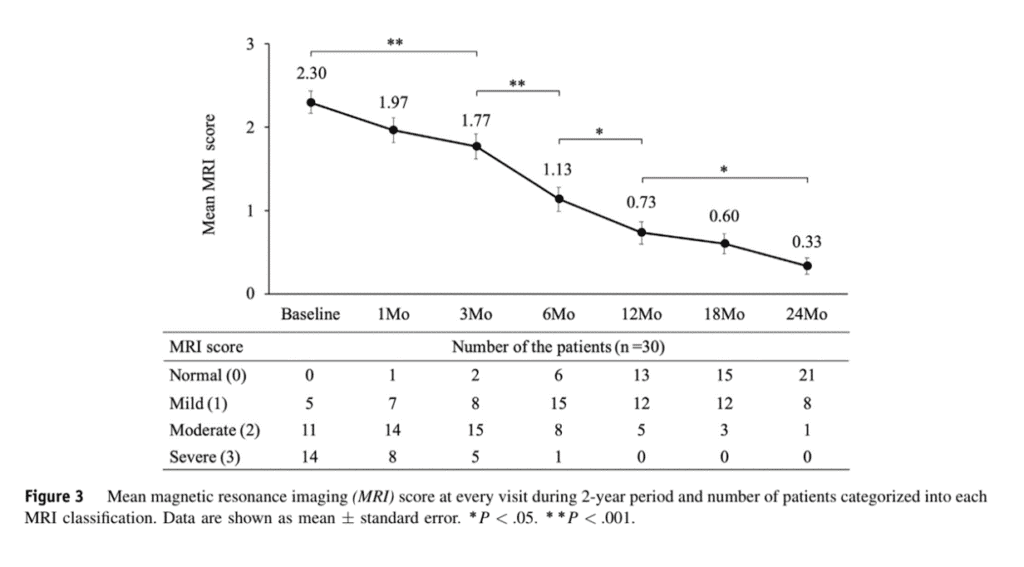
Credit: Suzuki et al
The mean MRI improvement scores are above showing a steady improvement in the tendon appearance on MRI over 24 months that correlated with patient-reported improvement.
One criticism of this study is that there is no control group that wasn’t injected, so it’s possible these improvements come from the natural resolution of the problem. However, that’s less likely as these patients had all failed at least 3 conventional nonoperative treatments (physical therapy, elbow straps, wrist splints, nonsteroidal anti-inflammatory medications, or corticosteroid injections) and they all had continuous symptoms for at least 6 months.
This Study is Not Unique
So is this type of objective tendon healing study using PRP unique? Nope. There is an even better research study with many more patients published in 2018 using MRI, a control group, and 7X PRP (4). In this study, which used similarly aged patients to the studies above, the PRP group showed better functional and MRI improvement, and this was directly correlated to the TGF-B levels in the PRP. This fits with our study showing that more concentrated PRP (which would have higher TGF-b levels) works better in this over 50 age group.
GF Levels and Tendon Healing
Platelets contain growth factors. These are contained inside alpha vesicles within the platelets and are released in a time-release fashion over about a week (5). These growth factors do what their name implies, they help various tissues grow.
How does the idea that higher PRP concentrations are needed to maximize results line up with a study like the one described above? After all, all patients were injected with the same preparation of PRP. The problem is that the amount of growth factors within each patient’s platelets is highly variable (6). Hence, even in a 7X PRP study, some patients will have enough TGF-b (a growth factor that helps tendon and other progenitor cells heal injuries) to maximize the effect and some will not. Hence, that’s why higher TGF-b levels in some patients link to better clinical and MRI results.
This wide variability in growth factor levels between patients has to be accounted for in clinical practice. That’s why our network physicians use 7-10X PRP at a minimum in aged patients and often get the concentration to 10-14X. That way, each patient, regardless of the TGF-b levels in their platelets gets over that minimum level required to maximize tendon healing.
The upshot? There is objective evidence out there that PRP helps tendons heal. That data fits with our published work on how platelet concentration in older patients is critical in maximizing healing in tendons. So the question every doctor must ask is what platelet dose am I capable of delivering using the simple bedside machine that I have? In the same way, every patient with a tendon problem should ask, what is the PRP concentration my doctor is capable of delivering? If you’re middle-aged or older, the answer should be at least 7-10X.
________________________________________________________________
References:
(1) Kearney RS, Ji C, Warwick J, Parsons N, Brown J, Harrison P, Young J, Costa ML; ATM Trial Collaborators. Effect of Platelet-Rich Plasma Injection vs Sham Injection on Tendon Dysfunction in Patients With Chronic Midportion Achilles Tendinopathy: A Randomized Clinical Trial. JAMA. 2021 Jul 13;326(2):137-144. doi: 10.1001/jama.2021.6986. PMID: 34255009.
(2) Berger DR, Centeno CJ, Steinmetz NJ. Platelet lysates from aged donors promote human tenocyte proliferation and migration in a concentration-dependent manner. Bone Joint Res. 2019 Feb 2;8(1):32-40. doi: 10.1302/2046-3758.81.BJR-2018-0164.R1. PMID: 30800297; PMCID: PMC6359887.
(3) Suzuki T, Hayakawa K, Nakane T, Fujita N. Repeated magnetic resonance imaging at 6 follow-up visits over a 2-year period after platelet-rich plasma injection in patients with lateral epicondylitis. J Shoulder Elbow Surg. 2022 Aug;31(8):1581-1587. doi: 10.1016/j.jse.2022.01.147. Epub 2022 Mar 2. PMID: 35247575.
(4) Lim W, Park SH, Kim B, Kang SW, Lee JW, Moon YL. Relationship of cytokine levels and clinical effect on platelet-rich plasma-treated lateral epicondylitis. J Orthop Res. 2018 Mar;36(3):913-920. doi: 10.1002/jor.23714. Epub 2017 Sep 20. PMID: 28851099.
(5) Martineau I, Lacoste E, Gagnon G. Effects of calcium and thrombin on growth factor release from platelet concentrates: kinetics and regulation of endothelial cell proliferation. Biomaterials. 2004 Aug;25(18):4489-502. doi: 10.1016/j.biomaterials.2003.11.013. PMID: 15046940.
(6) Cho HS, Song IH, Park SY, Sung MC, Ahn MW, Song KE. Individual variation in growth factor concentrations in platelet-rich plasma and its influence on human mesenchymal stem cells. Korean J Lab Med. 2011 Jul;31(3):212-8. doi: 10.3343/kjlm.2011.31.3.212. Epub 2011 Jun 28. PMID: 21779198; PMCID: PMC3129355.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
