Kneecap Arthritis Stem Cell Injection: Level 3 Orthobiologics Injection Knowledge
Yesterday I wrote about a way to determine how sophisticated your doctor is or isn’t in using things like platelets and stem cells. I showed you a simple level 2 issue that I had to correct before treating a patient’s knee with stem cells. Today we’ll cover a level 3 technique. All of this is to educate you about quality, as the most ethereal thing in medicine is figuring out if you’re getting the highest quality care possible.
The Orthobiologics Injection Scale
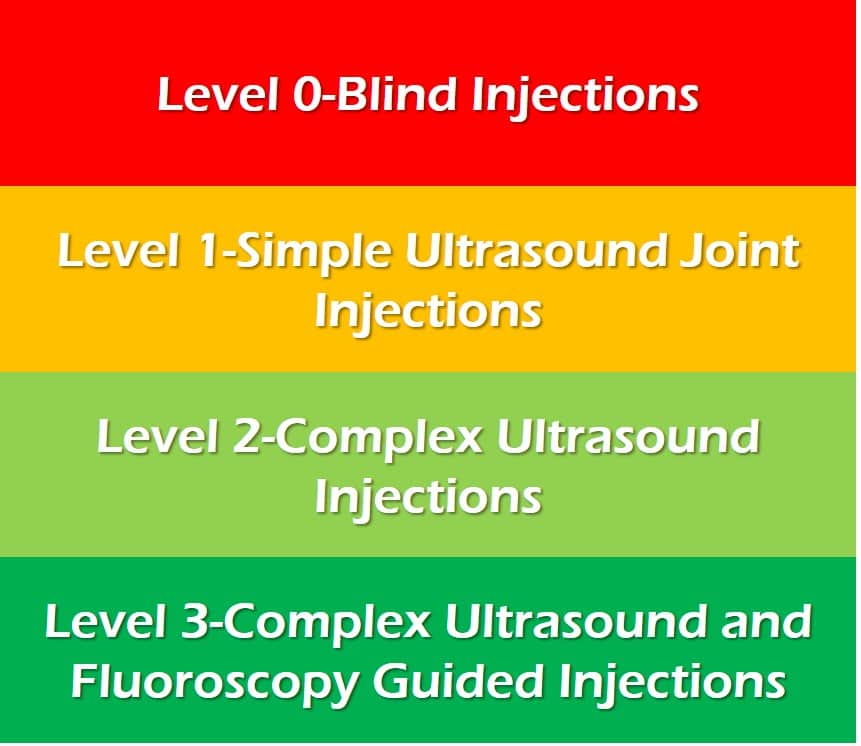
This is a scale I have used before that starts with blind injections and goes through simple and complex ultrasound and then ultrasound and x-ray guided procedures. It’s not perfect, as it’s possible to have ultrasound and fluoroscopy (real-time x-ray) in the office and have no idea how to use either. However, by giving you some examples of high-quality care, hopefully, you’ll be able to tell if that’s what’s being proposed for you.
A Problem Kneecap
Several of the patients I’m seeing this week at our licensed advanced culture site in Gand Cayman have lost cartilage on the backside of their kneecap (patella). One way to treat these patients would be just injecting stem cells into the joint and hope they make it to where you want them to go. However, there’s a basic science research study from back in 2008 that looked at how well cartilage repair with stem cells worked based on how you injected the cells. Turns out, if you place the cells directly on the cartilage lesion, you get better results.
In this study, the authors used bone marrow mesenchymal stem cells that were culture-expanded, just like the ones I’m using in Cayman. They either injected all of them into the joint or dripped those on a cartilage lesion. The second technique depended on a unique property of MSCs-they love to stick to surfaces. In this case, the goal was to get them to stick to the part of the knee that had the most cartilage damage. The authors showed that this worked well with about 80% of them attaching to the right spot in ten minutes. This is called a gravity-dependent attachment technique and this group also had the best cartilage repair results.
However, there’s a problem with these patients who have a cartilage lesion on the back of the kneecap. How can you get cells to attach there? That’s something that, believe it or not, has taken many years to perfect. Let me explain.
The Superman Injection Technique-Level 3 Knowledge

Many years ago I came up with a way to inject the backside of the knee cap and use gravity to adhere the cells just as in the study discussed above. We place the patient face down in “superman” position and offset the knees so one can be x-ray’ed in lateral position (see above). As you can see in the left lower picture, I then take the knee cap and pull it outward and place the needle on the backside of the patella (right picture). The top pics are the x-ray images demonstrating that the contrast (darker areas) is going where I want the stem cells, on the backside of the kneecap.
All of this might seem like commonsense and easy, but it’s been surprisingly difficult to perfect. Meaning it’s easy to place the needle in the wrong spot, to try this from the other side (medial-which doesn’t work), or have the contrast (the stuff I can see on the x-ray that will predict where the stem cells will flow) go to the wrong place. However, now it’s dialed in.
Also, realize that there is no textbook for these types of injections. Meaning, we have had to develop many of them from scratch. For example, before the concept of stem cells adhering to a surface, it just didn’t matter where you decided to place steroid or anything else injected into a joint. So these procedures are all brand new. In fact, I helped form a non-profit to teach these skills called the Interventional Orthopedics Foundation or IOF.
Why Not Just Do This with Ultrasound?
The problem with using ultrasound here is that there is no way to see where the cells will go. Small changes in where you place the needle can have drastic impacts on where cells end up. The bottom line is that ultrasound can’t see through the kneecap, while fluoroscopy can.
The upshot? Level 3 techniques in orthobiologics require both ultrasound and fluoroscopy. In addition, as you can see, these technologies require new ways of thinking about how physicians approach injections.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
