Making Cartilage Better on MRI
Mesenchymal stem cells (MSC’s) are a precursor to chondrocytes. This means that they can change into cartilage cells. The research on cartilage repair using MSC’s has exploded in recent years. A National Library of Medicine search this morning reveals over 1,000 research papers on the topic. While you may be surprised, when it comes to cartilage repair using MSC’s, we know quite a bit. We began treating joints with a simple BMAC and platelet derived mixture in late 2005. We published one interesting hip result, but didn’t see enough consistent results to warrant further investigation. This made sense, as the medical literature on BMAC wasn’t all that promising for cartilage repair. As a result, we switched to using culture expanded mesenchymal stem cells and began to see results.
To ensure that what we were seeing wasn’t simply a placebo effect (the patient wanting to get better so badly that he or she would claim improvement even though there was none), we enlisted the help of a local imaging center with the most powerful MRI magnet in production (GE 3.0 T). This MRI was 2-4 times more powerful than most in use. We spent years in IRB approved studies refining techniques, and this morning a case or two from that research database will help the reader understand joint cartilage. ED is a 58 year old female with a several year history of severe groin pain. She went to an orthopedic surgeon who obtained an x-ray showing hip joint arthritis and was told that she needed hip replacement surgery. She has recently lost >100 pounds from a gastric bypass surgery and was loving her new more active life, so the idea of having someone put in a prosthetic hip didn’t sit well. She found our research study and was accepted for a pre-op MRI. Low and behold, while the MRI showed the arthritis, it also showed a huge iiliopsoas bursitis. This meant that the lubricating sac in the front of the hip was swollen and could be the cause of her pain. As part of the study we needed a diagnostic block, basically a numbing shot to confirm where her pain was originating. We numbed her hip, but only some of her pain went away. So much for the need for hip replacement. We then numbed her swollen bursa and sure enough, most of her hip pain went away. So we treated both areas with MSC’s, the bursa and the hip. Her 15 month follow-up MRI (taken this month) shows no return of the bursitis and her groin pain is no longer present. What’s also interesting are the cartilage changes in her hip joint. The MRI images below are Fast Spoiled Gradient Recall Echo (FSPGR). They have been used in the research to help identify the quantity and health of cartilage.
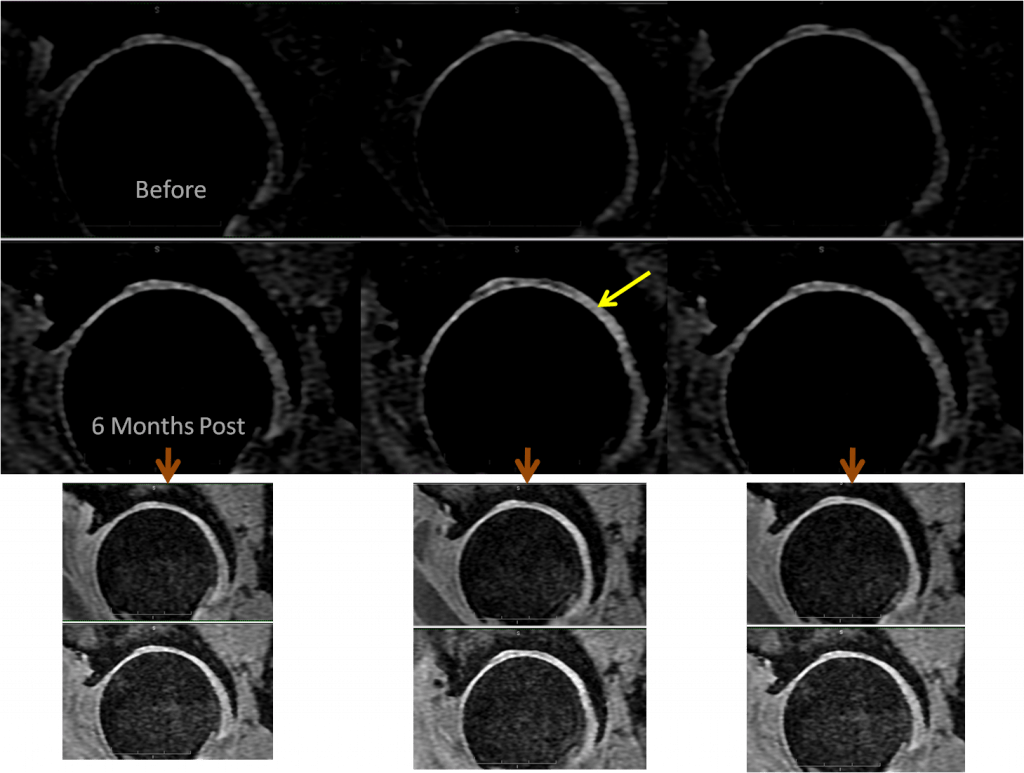
The most interesting part of this image is the change in the brightness of the cartilage. The cartilage is the white layer (yellow arrow) on top of the much darker “ball” of the femur. Since these are indentical image sequences taken on the same scanner, we can make this comparison. What does in mean when taken with her reports of improvement? We believe it means that there is more cartilage to produce MRI signal and that this cartilage has more water content (a good thing). Cartilage has GAG’s (gycosaminoglycans) that help it hold onto water. When these GAG’s start to leave the joint, the cartilage dries out and degenerates.
A second case that’s also important is that of a 38 year old man with cartilage loss in his knee from military training. A similar type of MRI image revealed:
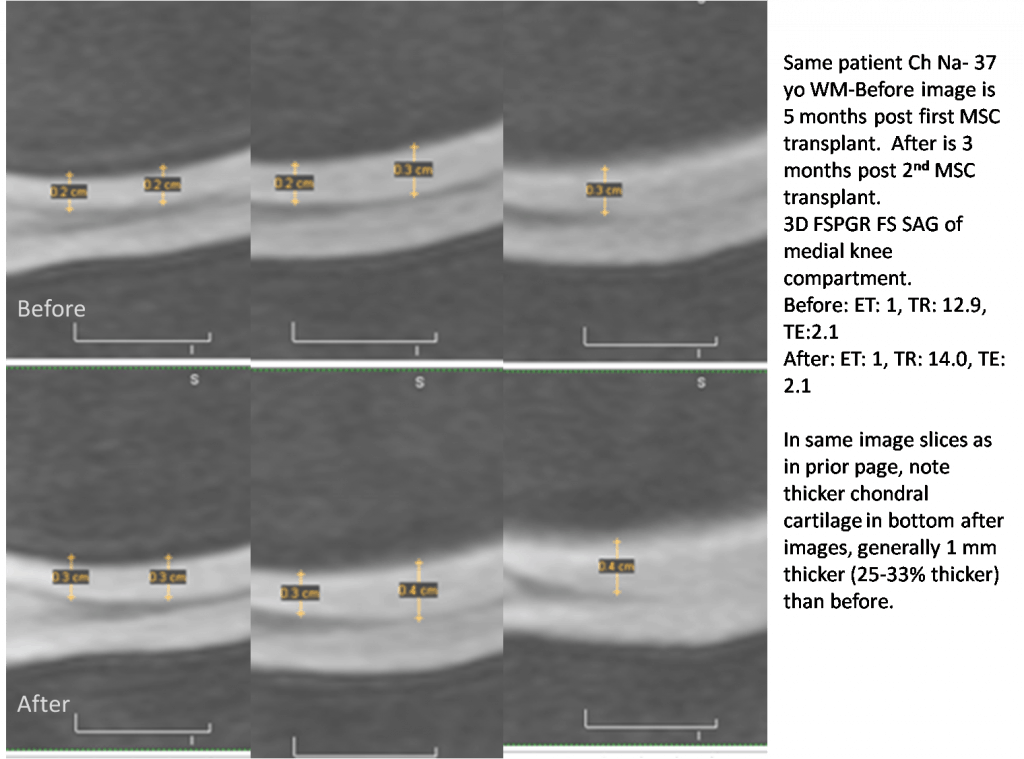
Realize that this is an extreme close-up of the cartilage on the femur bone of the knee. The blacker areas represent the bone and the bright areas the cartilage. There are many images slices because MRI marches across an area (in this case these are sagittal). In this patient’s procedure, the MSC’s were implanted along this cartilage surface. This pre and 5 month post procedure MRI shows between 25-33% thicker cartilage.
This patient was treated with the Regenexx-C (cultured stem cell injections).
Does every patient get more or better cartilage? We don’t have very large numbers of pre and post MRI’s, so we can’t say with any accuracy. What we can say is that we have seen MRI evidence of this happening and have even published some of these case reports (the two cases above are unpublished at this time). Here’s one published case study of meniscus regeneration measured by an imaging software program. Here’s another on repair of chondral cartilage (the cartilage on the end of the femur). We are also working on a much larger knee/hip joint research case series from our early commcercial experiences.
Originally published on

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
