How Does Muscle Recovery Work?
You may think you know how muscle recovery works, but things like creatine and rest are just the basics. There’s new research that shows it’s a bit more complex and interesting. Let’s dig in.
Scarring and Fatty Degeneration
There are two things that can happen to muscles during muscle recovery that cause big problems: scarring and muscle atrophy. When muscle scars, fixed fibrous tissue replaces the normal muscle fibers that can contract and relax. When it atrophies, fatty tissue replaces the muscle fibers. Either way, you end up with a dysfunctional muscle. One that’s either too tight or too weak.
Positive Versus Negative Control
My brain always goes to the idea that the body uses positive control. Meaning that it turns on the bad processes in response to the right circumstances. But it turns out that the body often uses negative control. Here it keeps the bad things at bay by inhibiting them. Remove the inhibition and all hell breaks loose. Turns out muscle recovery is more of a negative control system. Let’s dig in.
How Does Muscle Recovery Work?
Use It or Lose It
An observation we all make as we age is “use it or lose it”. We see this lack of muscle recovery all around us in the elderly. If they stop exercising, they rarely return. Stop walking and their ability to walk is permanently impaired. Stop getting up to walk and they become wheelchair-bound.
So how does that impact your muscle recovery and health? It’s also “use it or lose it” when it comes to the negative control system on scarring and fatty atrophy. It’s all about keeping the Fibro-adipogenic progenitors (FAPs) at bay.
FAPs – Good or Bad Depends on the Stimulus
Fibro-adipogenic progenitors (FAPs) can be bad boy cells. When they get activated, they cause muscle scarring or fatty atrophy. How much damage they do all depends on the stimulus.
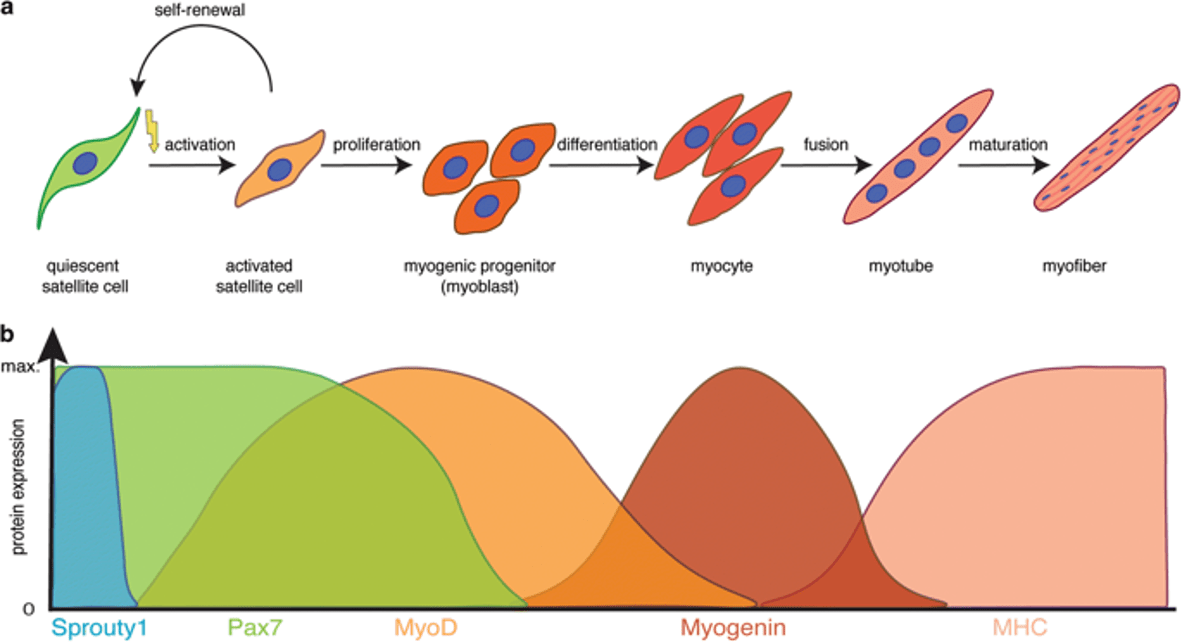
Routine damage to skeletal muscle, whether due to chemical or mechanical stress (a big workout), triggers a transient period of FAP activation and growth. This type of acute injury also causes satellite cells to become new muscle cells. When the acute inflammation returns to the baseline, the activated FAPs die off and are removed by the body. All of that constitutes normal muscle recovery
However, chronic inflammation causes a different story to unfold. FAP activation and proliferation are maintained at high levels. The activated FAPs aren’t killed off and removed by the body but stick around to cause muscle fibrosis and fatty atrophy. Muscles get scarred and weak.
The Impacts of Exercise on FAPs
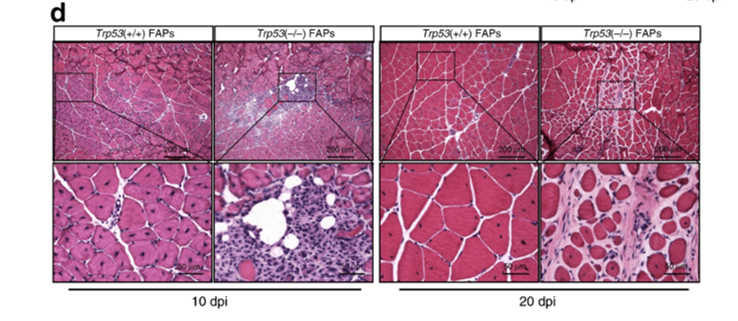
The new research used mice with both normal and diseased muscles (1). They were able to regulate the senescence (death) of FAPs with exercise. Exercise-induced muscle damage was effective for promoting muscle regeneration and promoting chronic low-grade inflammation. Meaning, exercise was key for muscle recovery.
Exercise was also found to get rid of the activated FAPs (through the senescence-associated factors p38 MAPK and NF-κB). Exercise promoted FAP cell death in normal mice, but an exercise program in muscle diseased mice did not work to get rid of FAPs unless the researchers intervened chemically. Then it worked well to promote normal muscle recovery.
In summary, in normal muscles, exercise creates acute inflammation due to small amounts of muscle damage. That causes a brief activation of FAPs. If you have too much chronic inflammation hanging around, like in metabolic syndrome (overweight, high blood pressure, high triglycerides), FAPs can stick around too long and can damage muscle. However, continued exercise will have a powerful effect on turning off the nasty FAP cells.
The upshot? Exercise is the key to maintaining healthy muscles. It stimulates satellite cells to promote new muscle growth and it inhibits the bad FAP cells that can cause scarring and fatty atrophy of muscles. Hence, exercise is the world’s best muscle recovery drug!
______________________________________________
References:
(1) Saito, Y., Chikenji, T.S., Matsumura, T. et al. Exercise enhances skeletal muscle regeneration by promoting senescence in fibro-adipogenic progenitors. Nat Commun 11, 889 (2020). https://doi.org/10.1038/s41467-020-14734-x

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
