Our Hip Arthroscopy Palooza Isn’t Going So Well
Medicalstocks/Shutterstock
If you read this blog, you know that I often write about what I experience as a doctor. This week a patient came in after Hip Arthroscopy asking if she should get a hip stem cell injection. I was appalled that nobody ever bothered to tell her that her surgery was highly likely to have a poor outcome based on her age and presence of osteoarthritis. That dovetails with new research showing just how poorly some of these patients do. Let’s dig in.
Hip Arthroscopy Palooza
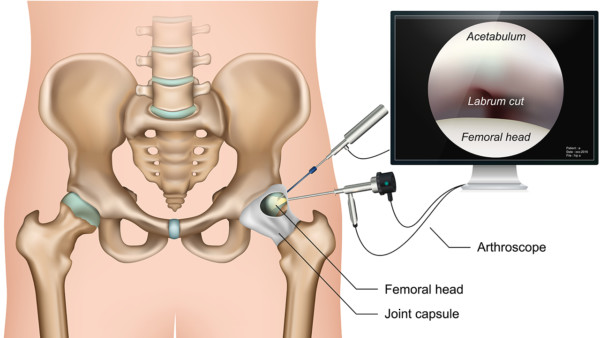
No single category of orthopedic surgery has exploded over this past decade as much as Hip Arthroscopy. Much of that surgery is built on the idea of hip impingement (FAI or Femeroacetabular Impingement). This is the concept that the hip develops bone spurs that restrict movement and cause excessive wear and tear and that it’s the doctor’s job to remove them. However, this story is sometimes more fiction than reality.
Take for example bone spurs on the socket part of the joint (pincer type). Surgeons love to remove these, but it turns out that the research shows that they form to protect the joint from more arthritis, so removing them makes no common nor scientific sense (1). Or take for example a recent study that showed that Hip Arthroscopy surgery to remove bone spurs was no better than no surgery (2).
The New Hip Research
Medical researchers recently reviewed more than 50,000 health insurance claims that involved Hip Arthroscopy (3). The number of Hip Arthroscopy surgeries doubled from 2010 to 2014. Even more concerning was that 1 in 5 patients who had hip arthroscopy surgery converted to either needing a second surgery or a hip replacement within 2 years.
Here’s the stunning part for my female patient in her 50s mentioned above. About 1 in 3 older patients (age 40-60) needed a hip replacement within 2 years! Ouch!
These results fit with other studies, for example one that analyzed seven studies with a total of 1,129 patients (4). The failure rate of FAI surgery was more than 8 times higher when the patient had any arthritis at the time of surgery. In addition, the percentage of people who needed a subsequent hip replacement was significantly higher in the FAI group with arthritis (37.3%) than in the FAI group without arthritis at the time of surgery (9.7%).
Why Didn’t My Patient Know This?
My patient had hip FAI surgery and microfracture at arguably one of the most famous hip surgery practices on earth. She had no idea that her advanced age and her pre-surgery arthritis put her at much higher risk that her Hip Arthroscopy procedure would fail. In fact, when I told her these things she was shocked. Why didn’t the surgeon drill these facts into her brain? Your guess is as good as mine.
The upshot? Hip Arthroscopy surgeries are being done on patients who either don’t need them or who are at substantial risk to do poorly. More concerning is that very little expanded informed consent happens in these patients. Meaning that they often have no idea that they are poor candidates for these procedures. Why?
_______________________________________
(1) Agricola R, Heijboer MP, Roze RH, Reijman M, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthritis Cartilage. 2013 Oct;21(10):1514-21. doi: 10.1016/j.joca.2013.07.004. Epub 2013 Jul 9. PMID: 23850552.
(2) Lodhia P, Gui C, Martin TJ, Chandrasekaran S, Suárez-Ahedo C, Walsh JP, Domb BG. Arthroscopic Central Acetabular Decompression: Clinical Outcomes at Minimum 2-Year Follow-up Using a Matched-Pair Analysis. Arthroscopy. 2016 Oct;32(10):2092-2101. doi: 10.1016/j.arthro.2016.04.015. Epub 2016 Jul 2. PMID: 27378389.
(3) Cevallos N, Soriano KKJ, Flores SE, Wong SE, Lansdown DA, Zhang AL. Hip Arthroscopy Volume and Reoperations in a Large Cross-sectional Population: High Rate of Subsequent Revision Hip Arthroscopy in Young Patients and Total Hip Arthroplasty in Older Patients. Arthroscopy. 2021 Apr 23:S0749-8063(21)00365-0. doi: 10.1016/j.arthro.2021.04.017. Epub ahead of print. PMID: 33901509.
(4) Lei P, Conaway WK, Martin SD. Outcome of Surgical Treatment of Hip Femoroacetabular Impingement Patients with Radiographic Osteoarthritis: A Meta-analysis of Prospective Studies. J Am Acad Orthop Surg. 2019 Jan 15;27(2):e70-e76. doi: 10.5435/JAAOS-D-17-00380. PMID: 30256340.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
