Reports of the Death of the C1–C2 Facet Injection Have Been Greatly Exaggerated
In 1897, Mark Twain was on a speaking tour in London when an American newspaper started a rumor that he was gravely ill. This was soon followed by an obituary. When asked by an American reporter in London about his death, Twain quipped, “The reports of my death have been greatly exaggerated.” I feel the same about C1–C2 facet injections. The radiofrequency mob has been trying hard to kill off cervical facet injections for years, and C1–C2 is low-hanging fruit, but like Twain, I have to report the death of this procedure has been greatly exaggerated.
What Is a Facet Joint, and How Does RFA Work?
Sometime around the turn of this last century, we began to see the use of radiofrequency ablation (RFA) for neck pain due to damaged facet joints take off. What is RFA, and what is a damaged facet joint?
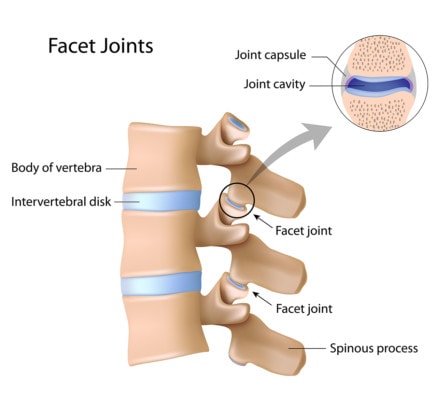
Alila Medical Media/Shutterstock
You have 14 joints in the back part of your cervical spine (7 on each side). These joints help to control neck motion. These little articulations, about the size of a finger joint, are commonly called “facet joints.” They can become injured or can get arthritis like any other joint in your body. When this happens, they can become chronically painful.
While the injection of anti-inflammatory steroids into these joints was the most common way to treat this pain, about the year 2000 or so, we began to see the rise of another form of treatment, called RFA. This procedure uses a probe that heats up to burn away nerves around the painful joint. The idea is that once these pain-carrying “wires” are “cut,” the pain will stop because it’s no longer being transmitted to the brain. This works pretty well and has been well researched to help chronic neck pain caused by a damaged facet joint. However, as you might imagine, you can’t just burn nerves that carry pain signals and not have consequences. This procedure can cause the joint to become more damaged (a Charcot joint) and, in my experience, can cause a cycle where the patient needs to be treated every 5–18 months forever. In addition, my personal observation is that these patients get more “brittle” with time. By that, I mean that when their pain returns, it’s worse and easier to provoke than before RFA was begun.
The RFA Biz Plan
Radiofrequency is a great medical business. Not only do these patients need to come back every so often for a repeat treatment, but insurance companies pay more for RFA than a simple facet injection. In addition, there’s a third-party vendor who gets to charge outrageous prices for disposable needles and new RF probes, which means that there’s lots of moolah around to sponsor conferences and pay physician thought leaders and medical directors. Hence, knowing that money talks in medicine, it’s not hard to figure out why those thought leaders have been trying to get rid of facet injections (i.e., injecting a substance into the joint rather than burning the nerves around the joint) as the idea competes with RFA. However, with the advent of orthobiologics, like PRP and stem cells, everything changes.
How Orthobiologics Upset the RF Applecart
My last RFA was done about a year ago. I went from performing several a week and hundreds a year to just a handful about five years ago. Why? Injecting PRP and stem cells into these damaged facet joints works just as well or better without having to kill important nerves. The same will surely happen in interventional-spine practices all over the world as PRP and stem cells gain insurance coverage for use in the spine. Which will create a big problem for physicians who bet the farm on RFA. First, like with any technological disruption, there will be financial winners and losers. However, there’s an even bigger problem. Most interventional-spine-trained physicians are losing their facet-injection skills. Nowhere is this truer than in the field of upper-neck-facet injections.
The Premature Demise of the C1–C2 Facet Injection
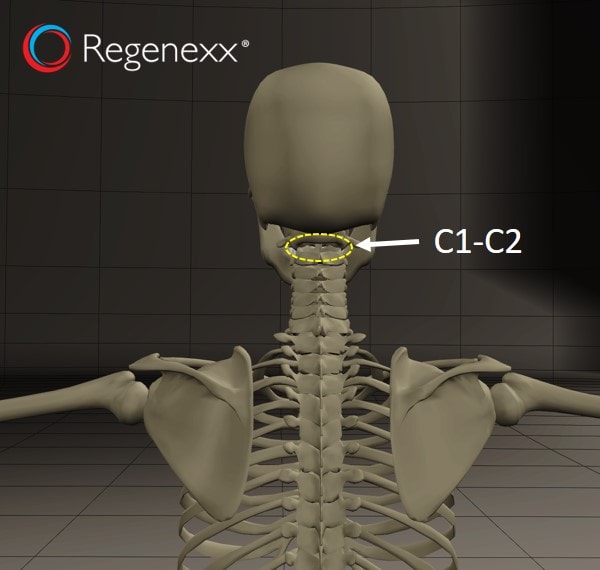
In patients with a chronic headache, the C1–C2 facet joint can often be a cause of pain. While the joint just below this can cause headaches more often, we’ve seen about a thousand patients over the last two decades who have headaches that are caused by the C1–C2 facet. While there are special risks in injecting this joint because an important artery that runs to the brain is close by, I’ve personally injected about 1,000 C1–C2 facets without any issues. Having said that, I always take this precise fluoroscopically guided joint procedure very seriously, as do many physicians.
A few years back, an editorial came across my desk. It turns out that a university-based physician had used the wrong procedure to inject a C1–C2 facet joint and used the wrong type of steroid and killed a patient. From reading the paper, it was clear that he put the needle where it didn’t belong, and in any neck injection, this type of inexperience can have disastrous consequences. Instead of recognizing that any injection performed the wrong way can hurt a patient, others published an opinion piece that suggested that we should give up injecting this joint.
The logical fallacy used by the authors of the editorial cited above is called a base rate fallacy. Basically, you point to an event where something bad has happened to focus the reader’s attention. However, you ignore the cases where nothing bad has happened, and you neglect to place the risk in context. The reader walks away believing that the event is representative of the risk as a whole when that’s really not the case.
Let’s use an automotive example to explore how ridiculous this conclusion is that C1–C2 facet injections should be abandoned. The author’s conclusion is similar to the celebrity exotic-car crashes we read about periodically in the paper. The reasoning goes like this. Since some celebrity crashed his Ferrari and killed someone, exotic cars are too dangerous and should no longer be sold. After all, the fatality rates in exotic cars are, on average, much higher than in, for example, a Toyota Prius. What this conclusion ignores is that there are many exotic-car trips where nothing happens. It also ignores the fact that while the celebrity can afford a new Ferrari, he may have no expertise in driving such a car. Hence, if we explore exotic-car crashes that happen on our highways further, we see that there are few such crashes when the car is driven by a professional or experienced driver.
While the paper above is based on a logical fallacy, it has had a negative impact on the number of upper-cervical-facet injections being performed. As a result of this publication and the general push toward RFA, it’s getting harder and harder to find physicians with much experience in precise C1–C2 facet-joint injections. In fact, I would estimate that we now have fewer than 50–100 US physicians who have injected more than 50 C1–C2 joints in their careers, which, IMHO, would be the minimum number of times to be able to claim any expertise in the procedure.
This is a real shame, as with orthobiologics set to replace RFA, the focus of interventional-spine physicians will shift from burning nerves to injecting substances into damaged joints to promote healing. In this world, the C1–C2 facet joint is a reasonable target to inject. In addition, if you consider that many of these patients with severe chronic headaches will end up on narcotics and the overdose death rate from these drugs is soaring, even the rare severe complication from the improper injection of this joint (like the example of the above physician who didn’t know what he was doing) will produce less morbidity than creating yet another oxycontin addict.
So What’s the Solution?
We need to be teaching more physicians how to inject the upper cervical spine safely, not dissuading them from injecting this area because it doesn’t fit the RFA biz plan and because some university-based yutz put a needle where it shouldn’t be. To that end, I will be constructing a course to revive these dying procedures, as with the orthobiologics wave beginning to get larger, we can save more patients from narcotic-induced deaths than will ever be harmed by this procedure!
The upshot? As physicians, we always need to look at what we do for patients and recognize when the business plan is driving the bus over what’s best for the patient. Why? The business guys in medicine will never do this, which leaves we physicians as the last line of defense for patients. So let’s be honest with ourselves. Is nuking neck nerves the best we can do for patients with damaged neck facet joints? Nope. It was a great idea for its time, but now it’s time to retire this invasive way to treat neck pain.
I leave you with another Twain quote:
“Whenever you find yourself on the side of the majority, it is time to pause and reflect.”

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
