Periacetabular Osteotomy: Should You Get Hip PAO Surgery?
You find out after a visit to the local orthopedic surgeon’s office that you or your young adult has hip dysplasia. One of the treatments offered is a surgery called PAO. You frantically search the Internet to figure out what that is and whether it’s a good choice. So today let’s explore hip PAO surgery. I’ll approach this as a physician educated in orthopedic research. Let’s dig in.
What is Hip Periacetabular Osteotomy?
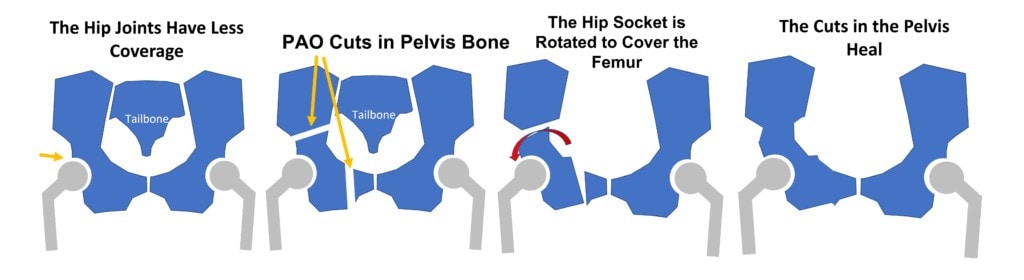
Periacetabular Osteotomy is also known has PAO surgery and involves sectioning and disconnecting one half of the pelvis and rotating the hip socket downward to treat a short socket (hip dysplasia) [see my illustrations above] (1). The idea is that the patient is born with a short hip socket and that this may cause hip arthritis at a young age (2). Hence, to reduce the need for an early hip replacement, hip PAO surgery is performed to cover the unprotected part of the hip.
While all of this sounds reasonable, let’s explore how much we know about this procedure. How invasive is hip PAO surgery? Should young people with hip dysplasia be lining up to get it?
My First Intro to Periacetabular Osteotomy?
About a decade ago, there just wasn’t all that much PAO surgery being performed. However, a patient called me wanting advice on whether stem cell injections could help her heal her PAO surgery caused pelvic non-union. Basically, for this patient, the cut areas shown above, never healed, leading to what doctors call a non-union. That meant severe pain with any activity causing the patient to be permanently bedbound. I have to say that I was floored when I understood that one-half of her pelvis (and therefore one leg) was permanently disconnected from the rest of the body. Shortly after that, a colleague called me with another patient who was more functional (he could get out of bed) and who also had a pelvic non-union (different surgeons) from a PAO surgery! Hence, my initial exposure to hip PAO surgery was not positive.
Hence, with that intro, let’s dive into what we know and don’t know about hip PAO surgery.
How Long Does Hip PAO Last?
This is the first and most critical question to ask about a surgery that’s meant to get rid of or delay the need for a hip replacement surgery. Meaning if you’re going to get half of your pelvis disconnected and then reconnected, how much additional time will you get before you need that hip replacement? Not as long as you would think given that this procedure is performed in young patients.
A recent large meta-analysis of many hip PAO research papers showed the percentage of patients who avoided a hip replacement (3):
- 75.9% at 10 years
- 36.5% at 20 years
So we have a very invasive surgery used in young patients meant to replace a hip replacement, but 1 in 4 patients who get the PAO procedure still need a hip replacement at 10 years and 2 in 3 still need one at 20 years?
If we had used a hip replacement later in life to treat these patients, on average let’s say in their 40s, how long would that prosthesis last? Based on one study for a specific polyethylene prosthesis, there would be a 96% chance of not needing a second hip replacement at about 22 years after the procedure (5). Meaning that it would be possible to have most of these patients only need two hip replacement procedures in their lives.
Could this math be off in some patients? Sure, some studies show shorter lifespans of varying hip prostheses and clinical scenarios.
Does PAO Surgery Work?
The medical standard to determine if a treatment works is a randomized controlled trial (RCT) where you compare it to something else or a placebo. In this study design, one group of patients gets the treatment you’re testing and the other group gets a different but standard treatment (like physical therapy or a placebo or sham procedure). So what does the RCT data say about whether PAO works? There have no such published data that I could find. Meaning at the end of the day, we have zero high-level evidence that this invasive surgery saves patients from a hip replacement. That’s critical because you would expect a 5-10 year study that looked at patients who got hip PAO surgery versus those who didn’t. That’s the only way that you can convincingly say that the surgery helped to reduce the need for a hip replacement. Any other study is considered “low-level evidence”.
Complications of Hip PAO Surgery
A meta-analysis of almost five thousand patients represented by 33 articles showed that the mean hip PAO complication rate was 14.1% or about 1 in 7 patients (4). That places hip PAO in the high-risk orthopedic category. For example, the complication rate of knee arthroscopy surgery is about 1% (6).
The Future of Hip Dysplasia Treatment
The concept behind hip PAO surgery is to reduce the need for a hip replacement in the age range of the 40s to 50s. Why does hip arthritis occur at these ages? Because of the ability for self-repair can no longer keep up with the added wear and tear of having a short hip socket. Hence, you can either reduce the wear and tear with surgery like PAO or just amp up the ability for self-repair as the patient ages. Given that orthobiologics like platelet-rich plasma, bone marrow concentrate, or culture-expanded mesenchymal stem cell injections may be able to help the joint last longer, it’s likely that hip PAO surgery will be replaced by a series of simple injections into the joint or bone or both (7-9) .
What Would I Do?
This is a tough choice for any patient or parent. Do you get a very invasive surgery to section the pelvis and re-attach it in the hope that you’re in the 1 in 3 that gets at least 20 years more time before needing a hip replacement? If the RCT research were clear that hip PAO worked dramatically better than doing nothing then it may be worth the risk. However, that research doesn’t exist. Hence I would favor periodic injections with orthobiologics to keep the hip as good as possible.
Jurassic Park and Science
If I had to come up with one summary statement after reviewing the research, that would have to be inspired by the original Jurassic Park movie. This is my favorite line from the movie:
That’s how I view PAO surgery. Just because it can be done, for most people, it doesn’t it make sense from a risk/benefit standpoint.
The upshot? As a physician who sees patients with hip pain all day, I am not impressed with the results of hip PAO surgery versus the risks. Perhaps we’ll have better research published, but so far the research into this surgery is of poor quality given the massive risk to the patient. Ultimately, I suspect as orthobiologics continue to improve, hip PAO surgery will eventually be relegated to the dustbin of medical history.
________________________________________________
References:
(1) Coobs BR, Xiong A, Clohisy JC. Contemporary Concepts in the Young Adult Hip Patient: Periacetabular Osteotomy for Hip Dysplasia. J Arthroplasty. 2015 Jul;30(7):1105-8. doi: 10.1016/j.arth.2015.02.045. Epub 2015 Mar 25. PMID: 25865812.
(2) Gala, Luca MD1; Clohisy, John C. MD2; Beaulé, Paul E. MD, FRCSC1,a. Hip Dysplasia in the Young Adult. The Journal of Bone and Joint Surgery: January 6, 2016 – Volume 98 – Issue 1 – p 63-73 doi: 10.2106/JBJS.O.00109
(3) Tan JHI, Tan SHS, Rajoo MS, Lim AKS, Hui JH. Hip survivorship following the Bernese periacetabular osteotomy for the treatment of acetabular dysplasia: A systematic review and meta-analysis. Orthop Traumatol Surg Res. 2022 Jun;108(4):103283. doi: 10.1016/j.otsr.2022.103283. Epub 2022 Apr 22. PMID: 35470119.
(4) Beck EC, Gowd AK, Paul K, Chahla J, Marquez-Lara AJ, Rasio J, Irie T, Williams J, Nho SJ. Pelvic osteotomies for acetabular dysplasia: Are there outcomes, survivorship and complication differences between different osteotomy techniques? J Hip Preserv Surg. 2021 Feb 5;7(4):764-776. doi: 10.1093/jhps/hnab009. PMID: 34377519; PMCID: PMC8349594.
(5) Parilla FW, Ince DC, Pashos GE, Maloney WJ, Clohisy JC. Long-Term Follow-Up of Conventional Polyethylene in Total Hip Arthroplasty in Young Patients: Heightened Wear-Related Complications Are Observed at the Beginning of the Third Decade. J Arthroplasty. 2022 Sep;37(9):1816-1821. doi: 10.1016/j.arth.2022.04.011. Epub 2022 Apr 21. PMID: 35460812.
(6) Friberger Pajalic, K., Turkiewicz, A. & Englund, M. Update on the risks of complications after knee arthroscopy. BMC Musculoskelet Disord 19, 179 (2018). https://doi.org/10.1186/s12891-018-2102-y
(7) Dall’Oca C, Breda S, Elena N, Valentini R, Samaila EM, Magnan B. Mesenchymal Stem Cells injection in hip osteoarthritis: preliminary results. Acta Biomed. 2019 Jan 10;90(1-S):75-80. doi: 10.23750/abm.v90i1-S.8084. PMID: 30715002; PMCID: PMC6503401.
(8) Mardones R, Jofré CM, Tobar L, Minguell JJ. Mesenchymal stem cell therapy in the treatment of hip osteoarthritis. J Hip Preserv Surg. 2017 Mar 19;4(2):159-163. doi: 10.1093/jhps/hnx011. PMID: 28630737; PMCID: PMC5467400.
(9) Singh JR, Haffey P, Valimahomed A, Gellhorn AC. The Effectiveness of Autologous Platelet-Rich Plasma for Osteoarthritis of the Hip: A Retrospective Analysis. Pain Med. 2019 Aug 1;20(8):1611-1618. doi: 10.1093/pm/pnz041. PMID: 30958873.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
