Potential Problems With Artificial Disc Replacement
On this page:
- Artificial discs and what they’re used for
- The problems with artificial disc replacement
- New research shows big complication rates
- A physicians experience with ADRs
Artificial disc replacement has been all the rage for the past 5 to 10 years. The idea is that it’s supposed to help reduce the side effects of bigger surgeries like fusion. Is that true? Are there problems with artificial disc replacement?
Artificial Discs and What They’re Used For
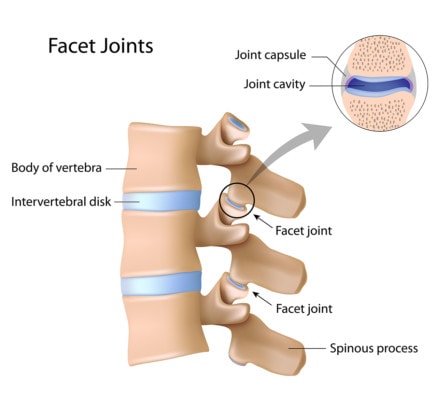
Alila Medical Media/Shutterstock
Your spine has discs between the bones that help absorb shock and control movement. Through wear and tear or injury, these discs can become degenerated and lose height. When that happens, the disc can bulge and irritate nerves, the facet joints in the back of that spinal segment can become overloaded and arthritic, and the segment can move too much (instability). This can lead to pain, nerve symptoms, and other problems.
Traditionally, patients with degenerative disc disease often underwent discectomy and laminectomy surgeries. That means that the surgeon removes part of the bulging disc and part of the bone around the spinal canal.
The problem with this procedure is two-fold. The removal of the disc material just weakens the disc, so there is a tendency for the disc to re-herniate. In addition, the removal of bone can make the segment more unstable. Hence, pain can return and when it does, that’s called a “Failed Back Surgery Syndrome.”
To try and fix these issues, surgeons began performing spinal fusion. The idea was that since pain is often caused by the degenerative instability and lost disc height, a spacer was inserted into the disc space to prop it up and hardware and/or bone was used to make that segment not move at all, then the pain would go away.
The problem? By making one segment of the spine not move, the forces the patient experiences just get shunted to another level which can get overloaded by too much force. Hence, while one problem is solved, another is created. This is called ASD or adjacent segment disease. To learn more, see my video below:
Because of these issues, artificial disc replacement (ADR) was created (see example below). The concept is that the device would allow motion and prop up the lost disc height. Hence, that should solve the issues with fusion. Right? Not so fast.
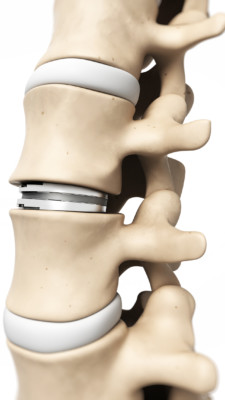
SciePro/Shutterstock
The Problems With Artificial Disc Replacement
So what does the research say that ADRs actually do?
- There is no difference between the outcomes of an artificial disc and a fusion (1,4).
- The way the vertebrae move is altered by ADR, meaning that the movement after surgery is not natural (2).
- There is no reduction in ASD when ADR is performed instead of fusion (3).
So the majority of the research not performed by the device manufacturers themselves or physicians on the company payroll don’t support the idea that ADR works any better than fusion.
New Research Shows Big Complication Rates
When one of my medical partners and I first began seeing patients show up with artificial discs, we both looked at each other and said with some irony, “What could go wrong?” After all, you’re taking something the size of a small hockey puck and inserting it into the spine. Now a new study answers that question.
The new study looked at a New York medical claims database to identify patients who underwent an isolated lumbar disc replacement surgery (5). A total of 1,372 patients were identified who had surgery between 2005-2013. The researchers then looked for subsequent surgeries after the ADR procedure. What did they find?
Almost 1 in 5 patients needed more surgery after lumbar ADR (17.6%). Almost 1 in 10 (8.8%) needed re-operation in the first two years. The only risk factor for needing more surgery was a patient with diabetes.
A Physician’s Experience With ADRs
I’ve been seeing disc replacement patients in the clinic now for decades. Based on what I see, most of these patients, like those who have had fusions, are coming to see me for new problems after ADR. Hence, I’m not a fan, based on what I have directly observed.
The upshot? Artificial disc replacements have their problems. Hence, at this point, my recommendation is to avoid spine surgery if all possible. In addition, there is no way to insert a small hockey puck in your spine without some collateral damage.
___________________________________________
References
(1) MacDowall A, Canto Moreira N, Marques C, et al. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease and radiculopathy: a randomized controlled trial with 5-year outcomes. J Neurosurg Spine. 2019;30(3):323-331. doi:10.3171/2018.9.SPINE18659
(2) Wachowski MM, Weiland J, Wagner M, Gezzi R, Kubein-Meesenburg D, Nägerl H. Kinematics of cervical segments C5/C6 in axial rotation before and after total disc arthroplasty. Eur Spine J. 2017;26(9):2425-2433. doi:10.1007/s00586-017-5073-z
(3) Yang X, Janssen T, Arts MP, Peul WC, Vleggeert-Lankamp CLA. Radiological follow-up after implanting cervical disc prosthesis in anterior discectomy: a systematic review. Spine J. 2018;18(9):1678-1693. doi:10.1016/j.spinee.2018.04.021
(4) MacDowall A, Skeppholm M, Lindhagen L, et al. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease with radiculopathy: 5-year outcomes from the National Swedish Spine Register. J Neurosurg Spine. 2018;30(2):159-167. doi:10.3171/2018.7.SPINE18657
(5) Perfetti D, Katz A, Job A, Galina J, Satin A, Silber J, Essig D. The incidence of subsequent lumbar spine surgery after lumbar disc arthroplasty: a minimum two-year follow-up. Spine J. 2020;20:S37-S38. doi:10.1016/j.spinee.2020.05.180.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
