Prolotherapy helps patient avoid the need for ACL replacement surgery
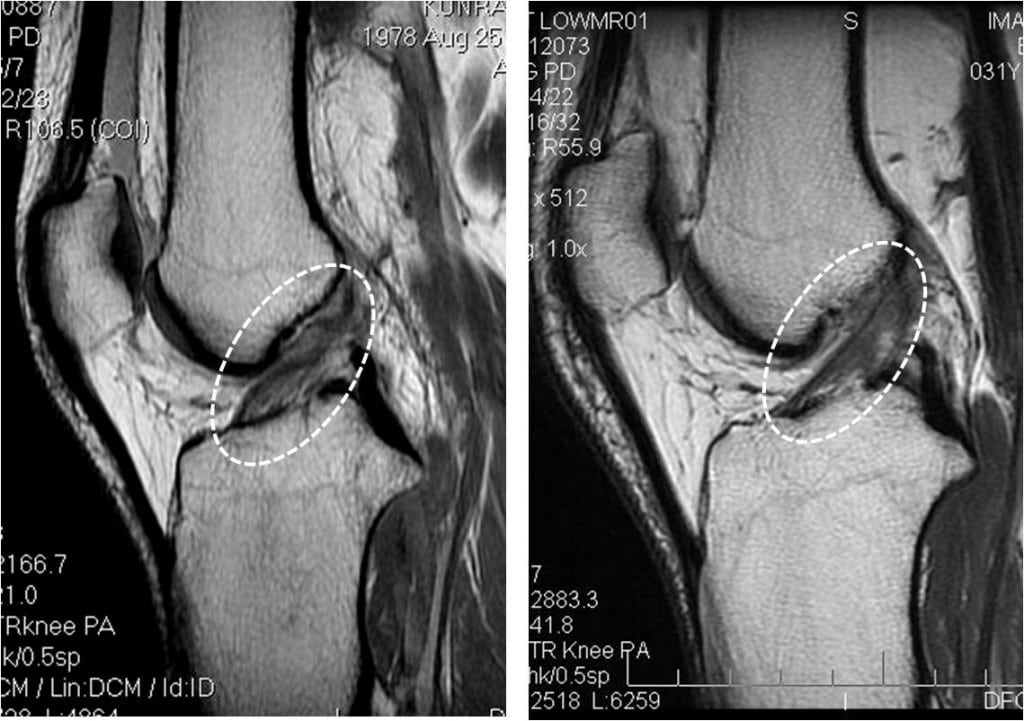
KL is an athlete in his late 20’s and an instructor at one of the military academies who injured his Anterior Cruciate Ligament (ACL). He was told he needed surgery to replace the ligament, but instead he sought us out for non-surgical options. We were glad to try and help, especially with the recent publication showing that repairing ACL’s surgically doesn’t prevent or change the onset of later arthritis. One option would have been a stem cell re-implant into the ACL under imaging guidance, but instead, we thought it best to try prolotherapy injections into the ACL under imaging guidance, as in our experience, in a young and active patient, this usually works to tighten the ACL. His pre-prolotherapy image is on the left above showing the ACL fibers as loose and poorly organized (in the white dashed circle, they meander upwards rather than appearing tightly stretched). The post-prolotherapy image is on the right, the ACL fibers are tightly arranged moving from the bottom left to the upper right. The fibers now appear to have a denser appearance (darker in this image). He reports better stability and less pain. I think this is a good example of how we approach knees. Our focus is to use whatever regenerative tools that work for the patient. For us, these include prolotherapy, PRP, advanced platelet preparations, or the patient’s own cultured stem cells. In this case, prolotherapy seems to have helped both the imaging appearance of the ligament as well as the reduced the patient’s complaints.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.