QC Kinetix Pricing: What Can We Learn from an Invoice?
I’ve blogged a few times about a clinic chain run by mid-levels offering low-level regenerative medicine care and charging top dollar. Today we’ll go over an invoice from that clinic chain, called QC Kinetix, and use that to learn about the differences between real clinical orthobiologics and an outfit built on sales. Let’s dig in.
An Invoice Posted Online
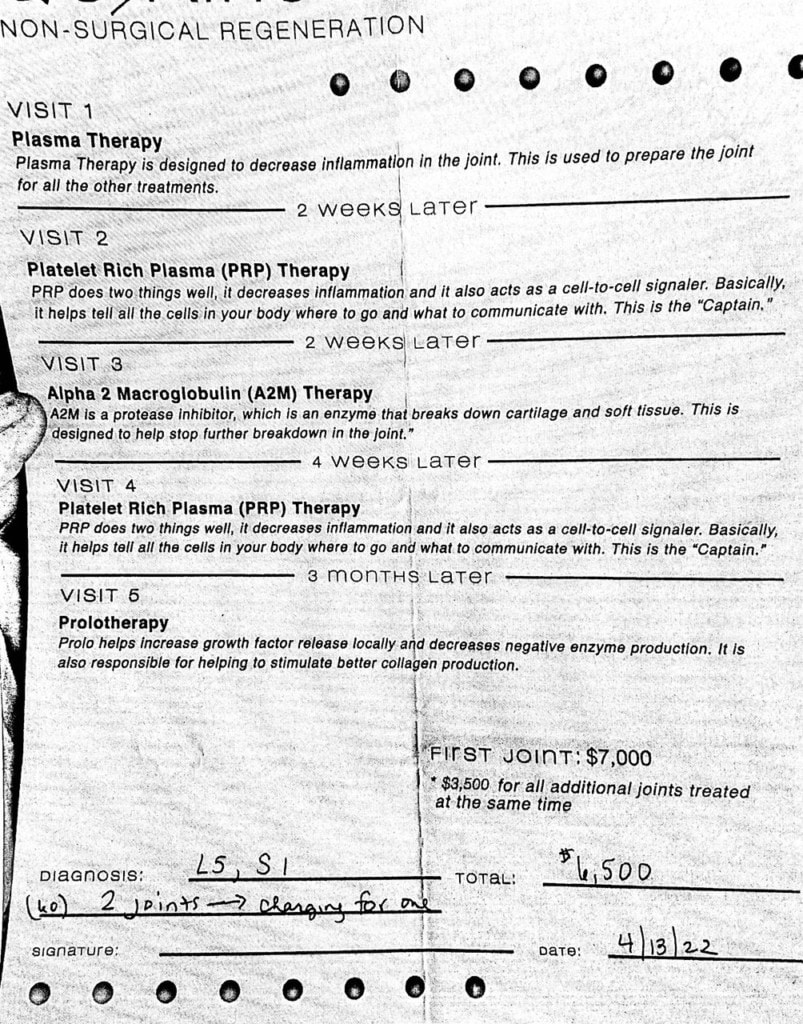
A physician in the Carolinas had a patient visit a local QC Kinetix franchise and then run to his office for an explanation of what QC wanted to do. The patient handed him the above form, which described treatment for his feet. This morning we’ll dissect this “treatment plan” to learn about the differences between a physician expert trying to help someone and a sales operation. However, before we do that, let’s get into what’s wrong with this patient.
A Linkedin Message
This patient’s doctor contacted me with the following message about the above bill:
“He’s a smart guy, and skedaddled outta there when he smelled the ________. But before he did they were able to come up with this boilerplate…plan within 10 mins of him stepping in the door.
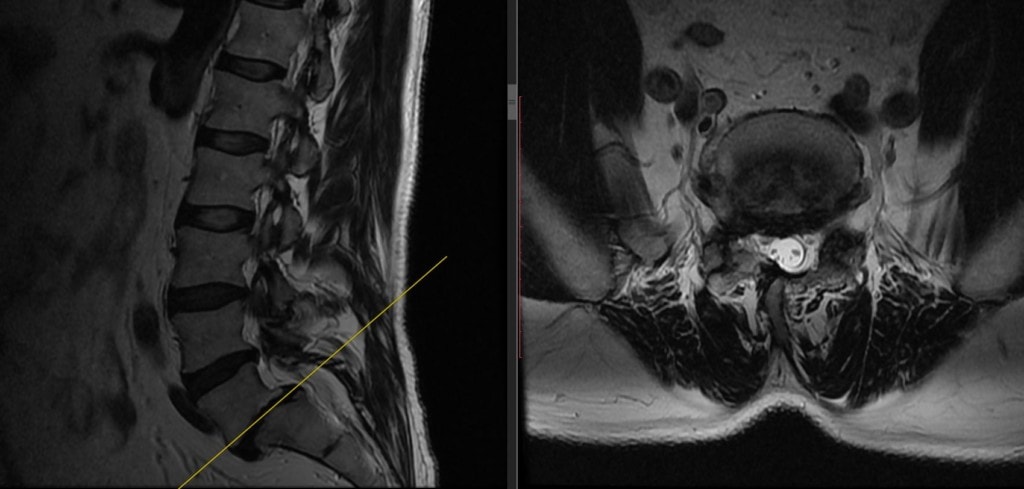
His complaints are basically “neuropathy” in the feet only, so exactly where they were proposing to treat is a mystery. I’m not even sure we will be able to help him….but he’s got beaucoup mechanical issues including L5 pars, spondylolosthesis, NFS, NR impingement at L5 and S1 so we may try to address those issues —- with minimal promises of improvement in “neuropathy.”
- Peripheral neuropathy
- Grade 2 L5-S1 spondylolisthesis
- Foraminal stenosis at L5-S1
- Facet osteoarthritis and hypertrophy at L5-S1
Going Over the “Treatment Plan”
On the invoice above is a treatment plan. That consists of:
- Plasma Therapy
- 2 weeks later, PRP
- 2 weeks after that, A2M
- 4 weeks later, PRP
- 3 months after that, prolotherapy
What does this treatment plan look like to an expert in this space? In my opinion, it’s nutty for many reasons. Let’s go over those.
First, the mantra who, what, why, and where applies. Meaning:
- Who will perform the procedure?
- What will be injected?
- Why is it being injected?
- Where will it be injected (which structure)?
As far as “who” is concerned, the physician subspecialist and the patient believe that the mid-level (NOT a doctor) is the one who would have performed the procedure. This is consistent with what I have seen from QC Kinetix. Is this appropriate for this type of patient who needs a spine procedure? Not in my opinion. The expertise required to treat a patient like this could only come from a highly trained physician super specialist in interventional spine who would have double the training of a mid-level (NOT a doctor).
What will be injected is detailed, but that brings up why it’s being injected. Let’s start with “plasma therapy”. What’s that? Is that “a thing” in spinal orthobiologics? Not really as that’s just taking the plasma from the blood. Meaning, searching the US National Library of Medicine for “plasma therapy lumbar”, there is nothing at all published. Next up is “PRP” therapy and that appears twice. That could help, but that depends on “where” as we’ll discuss below. “A2M” is a therapy that isolates the larger plasma proteins, one is A2M (alpha-2-macroglobulin) which may be able to help reduce cartilage breakdown, but used in this context of this patient and this level of basic injection care, makes no sense. Meaning this might be helpful if the provider performing the procedure was interventional spine trained physician who could place this accurately into the arthritic facet joints at L5-S1, but that’s not what’s being contemplated here (see below). Finally, prolotherapy can be helpful in tightening ligaments, which is consistent with what a mid-level (NOT a doctor) could do with a simple blind or ultrasound guide injection.
There’s also another side here to “why”. This patient has come into the clinic to get his neuropathy treated. While that could have something to do with his low back nerves being irritated by the spondylolisthesis (slipped vertebra), it may have nothing to do with it at all. Meaning that injecting this stuff at “L5-S1” may have ZERO effect on his neuropathy symptoms.
Finally, we come to the biggest issue with this treatment plan, where will all of this stuff be injected? Again, a highly trained interventional spine expert using fluoroscopy guidance could inject the following structures:
- L5-S1 facets
- Epidural space at L5-S1 (preferably transforaminal)
- The atrophied multifidus muscles
- Specific ligaments like the iliolumbar, supraspinous, and interspinous
However, a mid-level (NOT a doctor) could only generally inject about half of these structures. Placing PRP in some of these spots could make sense, as long as we knew that this guy’s neuropathy had something to do with his low back problem. We have no data that A2M or plasma will help. Prolotherapy could help, but in my experience, once the slipped vertebra gets this bad, it usually doesn’t move the needle.
Candidacy and Timing
What the invoice above fails to tell us is whether this guy is a Good or Poor candidate for this treatment. If I were seeing him in the office and with what his physician specialist relayed, neither of us feel that it’s more likely than not that his peripheral neuropathy could be helped with any platelet or blood-based treatment plan. Meaning rather than the “hard sell”, he would get the opposite. We would caution him that his chance of having the numbness in his feet go away with our treatment of his spine is less than 50/50. As a result, he may choose not to get treated at all.
Finally, the timing of these treatments is, in my opinion, bizarre. Meaning that in our clinics, he would get an initial trial treatment with platelet-based therapy in all of the spots discussed above, and then we would wait 4-6 weeks to make sure he had a response before even offering him a second or subsequent treatment. That’s because there is a significant and reasonable doubt that he can be helped. Jamming a bunch of treatments into that first 6 weeks is more likely than not to cost more and expose the patient to more risk.
Hard Sell
As I’ve written before, a big concern is that QC Kinetix employs professional salespeople who upsells from a basic form filled out by a mid-level (NOT a doctor). In my opinion, this is a serious problem from a medical standpoint as the medical treatment plan is usually fixed in stone based on a risk/benefit analysis. Meaning, that while adding procedures to the patient’s plan may maximize clinic income, that’s usually not medically appropriate.
The upshot? This is what I have come to expect from QC Kinetix. In my opinion, this is an aggressive sales outfit that runs clinics staffed by mid-levels (Not a doctor). I’m glad this patient got the vibe of the hard sell and ran out the door. My concern is for all of the patients that never figure that out.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
