Removing Hip Bone Spurs in Hip Impingement Surgery No Better Than Doing Nothing
Hip impingement as a diagnosis freaks people out. They can envision that bone spurs on their hips are wearing away cartilage with every single move. It’s a horrifying idea. This is despite many studies showing that loads of patients without hip pain have all sorts of MRI findings that a surgeon would operate on if they did have pain. Now a new study shows just how worthless surgery to remove those dreaded bone spurs can be—unless you’re a surgeon and you likely still think the results are pretty great. Let me explain.
Logika600/Shutterstock
Removing Hip Bone Spurs Has Launched an Entire Industry: Hip Impingement Surgery
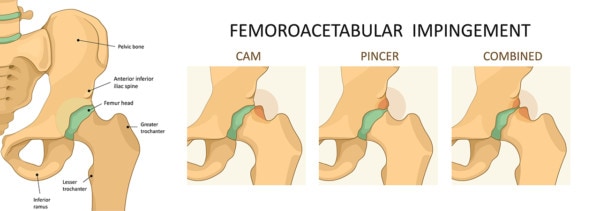
Hip impingement surgery is huge business. Fifteen years ago the surgical options for patients with hip pain were limited to a hip replacement. Then arthroscopic surgery came to the hip, and it created a whole new field of orthopedic surgery. The real driver of the now-common surgery is hip bone spurs and impingement. The idea is that there are bone spurs (extensions of the normal bone due to wear and tear) that grow and cause the hip joint to become impinged. The idea is that these extra pieces of bone press on the cartilage and wear it down, leading to arthritis. This is a horrifying thing for a patient to think about—every step is killing my cartilage! The problem is that the idea is mostly B.S.
The Chicken or the Egg Problem in Hip Impingement Surgery
The big question, or inconvenient truth, that hip surgeons tend to ignore is what came first—the bone spur or the arthritis? Meaning is the bone spur forming because of the arthritis, or is it causing the arthritis. If it’s the former, then removing hip bone spurs makes little common sense. If it’s the latter, then maybe removing it is a good idea.
Take, for example, the spurs that form off of the hip socket, also called the acetabulum. These are also called pincer spurs or a pincer deformity. The hip surgeons love to lop these off because studies have shown them to be “associated” with arthritis. However, association is not causation. Meaning, for example, that cigarette smoking and coffee drinking are associated in many studies with lung cancer; however, in other studies designed to determine what causes lung cancer, only cigarette smoking is found to cause lung cancer. Turns out that coffee drinking is just a casual observer since many people love a cup of Joe with their cigarette.
In the case of the hip-socket bone spur (a.k.a. pincer deformity), turns out in studies designed to see what causes what, the bone spur is actually forming to protect the hip joint from arthritis. Meaning, over time, people who develop these spurs have less and not more arthritis. Hence, removing this spur in most patients is not a good idea.
The Most Recent Hip Socket Bone Spur Removal Study
The orthopedic research is awful. I’m not the only one that thinks that, as one of my favorite British Medical Journal editorials states that the state of orthopedic research is “scandalously poor.” First, what a great British term! We verbally challenged Americans would never come up with such a great way to describe that the orthopedic research is awful.
This new study evaluating the effects of removing hip bone spurs in Hip Impingement Surgery is a great example of why the orthopedic research is scandalously poor. In this study the authors looked at 49 hip surgeries where the spur on the acetabulum was “whacked off” versus 147 patients who were similar but who had no surgery. While the patients were all very satisfied with their surgeries and reported that the procedure worked well, so did the patients who didn’t get the surgery! Huh? How is that possible? These poor patients had an awful and evil spur that was slowly draining the life away from their hips. Why was doing nothing as good as removing hip bone spurs surgically? See above. The spur was there to protect the hip, not to wear it away.
The most hilarious thing about this study is that despite the fact that the authors couldn’t prove the surgery did anything, they concluded:
“This study showed that patients with a CAO treated with CAD during hip arthroscopy had favorable outcomes at minimum 2 years postoperatively. Furthermore, the study group showed similar PRO scores and VAS to the control group. We conclude that CAD is a viable treatment option for CAO, yielding clinical improvement at short-term follow-up.”
In plain English:
“This study showed that patients who had their hip bone spurs removed in Hip Impingement Surgery reported good results. Furthermore, there was no difference in the results between patients who had the surgery versus those who didn’t. We conclude, therefore, that our surgery works well.”
Huh? In any other field, the title of this paper would have to be, “Removing Hip Bone Spurs Doesn’t Work,” spruced up, of course, in medicalese so that patients could barely understand the terminology. So now do you see why that British author firebombed the orthopedic research?
The upshot? Based on the two studies discussed here, removing hip bone spurs in Hip Impingement Surgery is mostly a folly (sneaking in another great British term there). This study showed that it didn’t add anything when compared to just doing nothing. Hence, if you’ve been told you have a hip socket spur, please don’t envision in your head that your every waking step is destroying cartilage. Instead, envision it as a warm and cozy safety blanket protecting your joint from further damage. Finally, don’t let anyone remove your safety blanket!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
