Should I Get Meniscus Surgery? Stop and Read This…
As you know, if you read this blog, the things I see in the clinic make up a good deal of what I write. This past week I saw a poor guy who was made much worse by meniscus surgery. It wasn’t hard to see why this happened. So if you’re considering meniscus surgery, let me share some research and then his story with you.
Should I Get Meniscus Surgery?
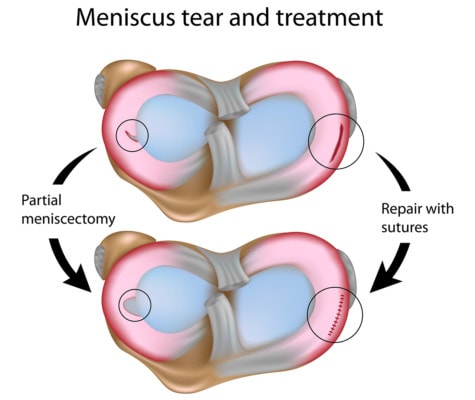
The meniscus is a shock-absorbing tissue that lives between the femur (upper leg bone) and tibia (lower leg bone) and functions as a cushion for the cartilage in the knee joint. Meniscus tears happen. If you are middle aged and don’t have meniscus tears, you are rare indeed. However, when orthopedic surgeons see meniscus tears on an MRI and the patient has knee pain, meniscus surgery is a common solution, so common, in fact, that in America it clocks in at about 700,000 surgeries a year. The problem with this is that middle-age people without knee pain are just as likely to have meniscus tears, so a meniscus tear shouldn’t be the assumed cause of knee pain. Despite this, it often is assumed, and surgery is performed. Of course, there are instances, as well, where a meniscus tear, such as a sports injury or a large tear, may actually be causing some pain. You may be thinking in cases like this, should I get meniscus surgery? Is meniscus surgery, in either case, at least fixing the knee pain?
It’s such a common surgery, you would think so; however, all of the high-level research to date shows that meniscus surgery is ineffective and it’s not helping pain any more than physical therapy. In fact, meniscus surgery is creating the perfect environment for the patient to develop arthritis in the future. Let’s talk about how a meniscectomy works (be sure to watch my video above for explanations using the stress ultrasound images).
On the surface, a meniscectomy might seem simple enough: A patient has some knee pain, an MRI shows a little tear in the meniscus (see video), the surgeon correlates the two, and the patient decides to have surgery. During surgery, the orthopedic surgeon will access the knee joint and whack out the torn piece of meniscus. This is where it gets more complicated—the meniscus tear may be gone after surgery, but so is a chunk of the meniscus, and nothing good can come of this. Let me explain.
Alila Medical Media/Shutterstock
The Problem with Meniscus Surgery
Think of the meniscus as a cork in a bottle. The cork is the right size and perfectly seated so that the pressure within the bottle won’t push the cork out. If the cork is too short, however, or unevenly seated, that pressure’s going to pop that cork out. The same thing happens with a meniscectomy. With a chunk of the meniscus missing, there is less meniscus to anchor it in the joint and the meniscus tends to push right out of the joint. When that happens, the meniscus no longer has the functional ability to properly protect the joint.
The knee images in the video above are from a patient who came to me eight months after meniscus surgery. During a stress ultrasound, as I stress the joint, everything is shown in real time, providing a vivid picture of the movement of the meniscus in the joint. In the video, you can see clear differences when I stress the patient’s normal knee and when I stress his surgery knee. On the surgery side, you will see his joint gape open and the meniscus being sucked into the joint and then pushing back out. This is joint instability and it’s making the patient miserable. It will also cause further issues down the line as it can increase wear and tear on the joint. This all falls in line with multiple high-level studies showing that chronic pain is the biggest reason patients give for dissatisfaction following meniscus surgery.
Do Not Get Meniscus Surgery! There Are Other Options
Hopefully, the video above demonstrating the results of addressing the situation surgically has answered the question, should I get meniscus surgery. Thankfully, surgical orthopedics isn’t the only option out there. In interventional orthopedics, the goal is to first determine the true source of the pain and then treat the source. If meniscus treatment is necessary, a nonsurgical approach using a precise ultrasound-guided injection of your own platelets or stem cells may help the problem.
The upshot? While there may be rare cases when meniscus surgery is still an option, in 2017, the evidence is clear that routine meniscus surgery is no longer appropriate. Just take a look at what happened to my patient’s knee joint as a result of surgery and what I see every day in the clinic.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
