Should I Have Surgery for Spinal Stenosis?
As a doctor who helps patients avoid spinal surgery, I get asked this question several times a week: “Should I Have Surgery for Spinal Stenosis?” The answer is frequently “No”, so let’s delve into why I think that and go over the results of one patient who we helped avoid the surgery.
What Is Spinal Stenosis?
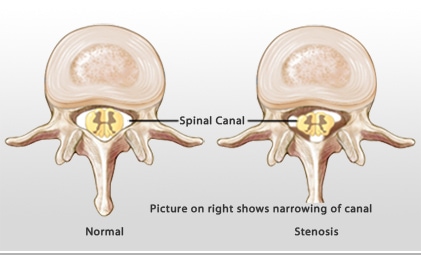
Before I answer the question, “Should I Have Surgery for Spinal Stenosis?”, let’s review the diagnosis. The term “stenosis” simply means a tight area. For example, you may have heard of coronary artery stenosis, which means a narrowed artery in the heart. Here the narrowing is in the spine. The spinal cord and nerves travel through holes in the bones called the spinal canal which the area we’ll be discussing.
What Are the Symptoms of Low Back Spinal Stenosis?
By far, the single biggest and most common symptom is the inability to stand for any significant length of time. Patients with central canal stenosis can usually measure their standing time in minutes. Meaning, they will commonly say that they can stand 5 to 20 minutes before they have severe back pain, numbness, and tingling, or weakness in the legs. When they sit down, all of this goes away quickly. They also to like to walk bent over, so for example, leaning over a shopping cart may feel more comfortable.
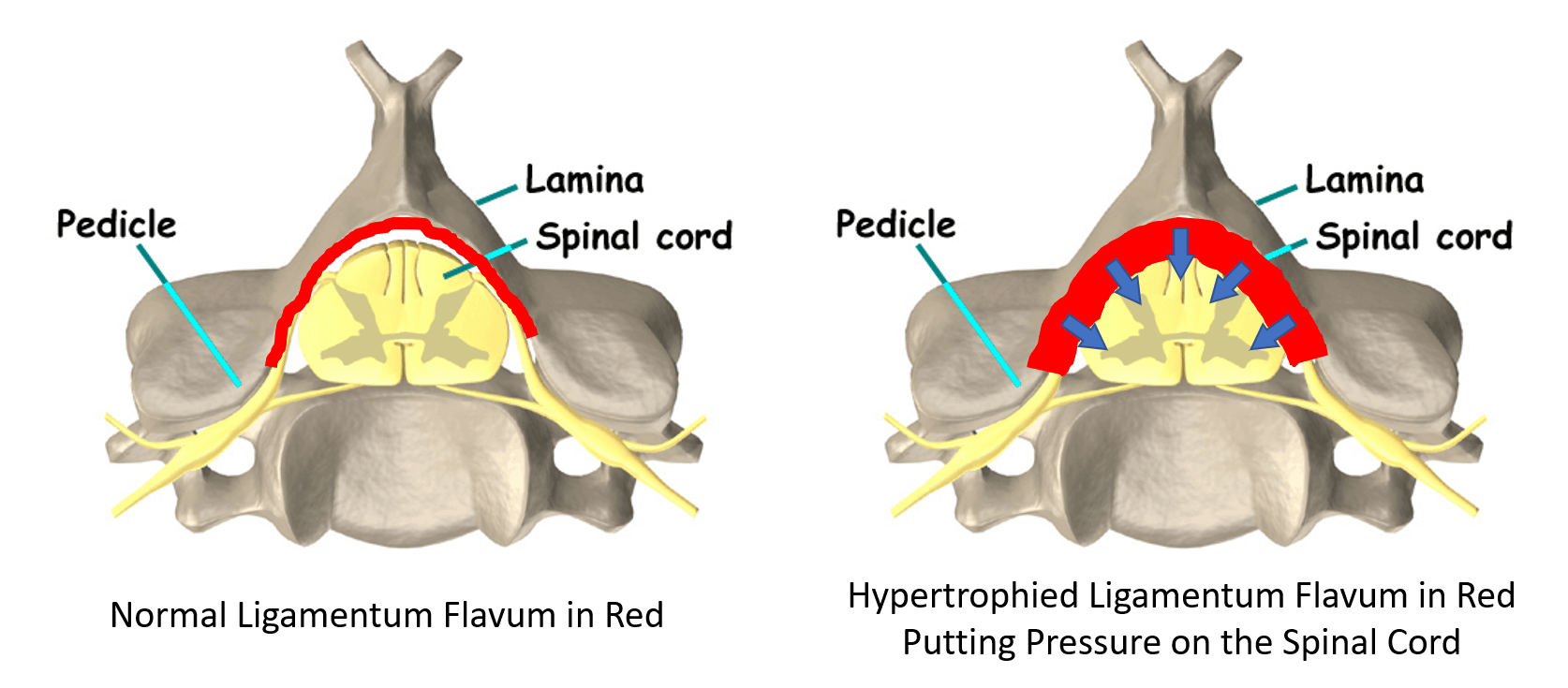
Why does this happen? To understand that we need to learn more about a ligament in the spine called the ligamentum flavum.
Meet the Ligamentum Flavum
To learn more about central canal stenosis, see my video below:
How to Make the Critical Decision, “Should I Have Surgery for Spinal Stenosis?”
While medications or physical therapy may help, once the spinal canal gets much smaller, surgery is often recommended (1). There are a couple of types of common surgeries:
- Decompression – The surgeon removes the bony back wall of the spinal canal and the ligamentum flavum and usually part of the facet joint to “open up” the area. A bulging disc may be shaved down.
- Fusion – The surgeon places screws, rods, and often cages where the discs go. This fuses the area solid so that nothing moves.
- Artificial discs – This is instead of fusion. This is where the surgeon takes out one or more discs and replaces them with a prosthesis.
Often decompression is performed with either fusion or artificial discs. The downside of both of these procedures is what’s called Adjacent Segment Disease (ASD). This means the area above and below the surgery will get too much force and begin to break down. See my video below to learn more:
Does the research show that surgery for stenosis works? Maybe in the short run, but in the long run several years after the procedure, patients are about the same whether they had the surgery or not. Or the surgery result is no better than just getting physical therapy (3,5,6). Won’t you get paralyzed if you fall or get in a crash? Regrettably, this is also a common misconception as the risk of the surgery usually exceeds the risk of spinal cord or nerve injury due to trauma (6,7).
Are there situations where someone definitely needs the surgery? Yes, if there is significant weakness in the hands or legs and less invasive therapy as described below doesn’t work, then the patient may need spinal surgery despite the possible side effects.
What Are the Risks of Surgery for Spinal Stenosis?
One of the reasons you may want to avoid spinal stenosis surgery is complications. To take a deeper dive into that subject, it’s good to understand that some of what spine surgeons report in research studies on complications is often very different from what patients report. Meaning that spine surgeons can underestimate surgery complications (2). For example, in a recent analysis, the complication rate of spine surgery was 10-24% (3). That’s 1 in 10 to 1 in 4 patients who got the surgery! Those complications included infection, nerve damage, more pain, or the need for more surgery.
If I Don’t Have Surgery, What Else Is Available?
We have been helping patients avoid spinal stenosis surgery for years by using their own platelets or stem cells. How does that work? Watch my video below to find out:
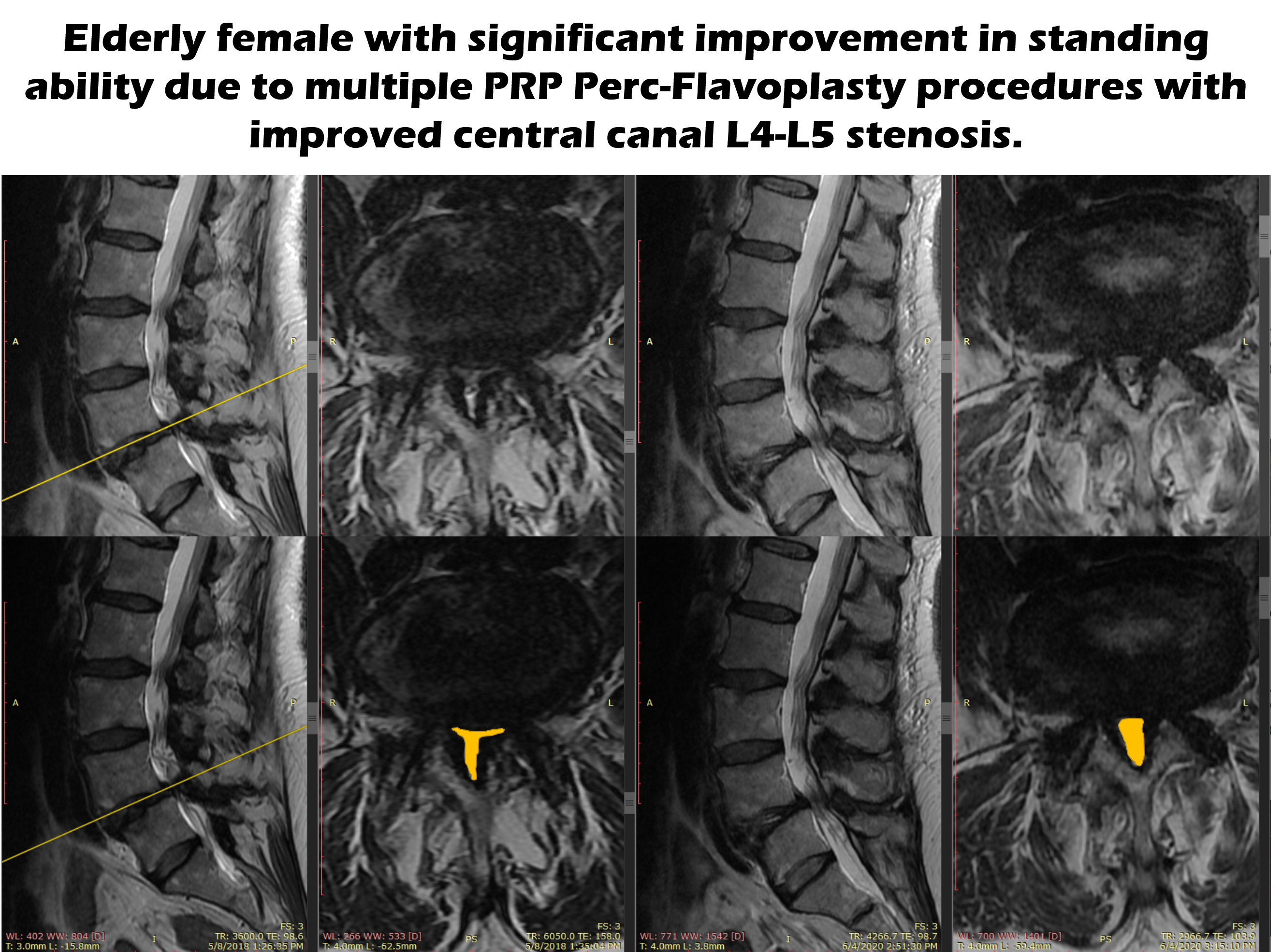
Does it work? Below are the MRIs of an elderly woman who we treated. The top row of MRI’s hasn’t been altered. On the left are the “Before” images and on the right are the “After” images. Since I know it’s tough for a non-physician to read these images, I have outlined the spinal canal in the images in the second row. As you can see, the size of that yellow area (the spinal canal) is smaller on the left before the procedure and much bigger after several procedures. This might not seem like a huge difference, but this difference helped this woman be able to stand again for more than an hour.
The upshot? Spinal stenosis is a common problem for many people as they age. The answer to the question “Should I Have Surgery for Spinal Stenosis?” is now different. These days there are non-surgical options. So think twice before a big surgery!
_____________________________
References:
(1) Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016 Jan 4;352:h6234. doi: 10.1136/bmj.h6234.
(2) Ratliff JK, Lebude B, Albert T, Anene-Maidoh T, Anderson G, Dagostino P, Maltenfort M, Hilibrand A, Sharan A, Vaccaro AR. Complications in spinal surgery: comparative survey of spine surgeons and patients who underwent spinal surgery. J Neurosurg Spine. 2009 Jun;10(6):578-84. doi: 10.3171/2009.2.SPINE0935.
(3) Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;2016(1):CD010264. Published 2016 Jan 29. doi:10.1002/14651858.CD010264.pub2
(4) Lurie JD, Tosteson TD, Tosteson A, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2015;40(2):63–76. doi:10.1097/BRS.0000000000000731
(5) Delitto A, Piva SR, Moore CG, Fritz JM, Wisniewski SR, Josbeno DA, et al. Surgery Versus Nonsurgical Treatment of Lumbar Spinal Stenosis: A Randomized Trial. Ann Intern Med. 2015;162:465–473. doi: 10.7326/M14-1420
(6) Cheung, Jason Pui Yin, and Keith Dip-Kei Luk. “Complications of Anterior and Posterior Cervical Spine Surgery.” Asian spine journal vol. 10,2 (2016): 385-400. doi:10.4184/asj.2016.10.2.385
(7) Murphy, Donald R et al. “Cervical spondylosis with spinal cord encroachment: should preventive surgery be recommended?.” Chiropractic & osteopathy vol. 17 8. 24 Aug. 2009, doi:10.1186/1746-1340-17-8

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
