Should You get Hip PAO Surgery?

What the heck is periacetabular osteotomy (Hip PAO surgery)? We have been concerned about the rapid rise in hip labrum and CAM impingement surgeries for FAI. However, this picture above tells a whole new story, one that moves our concern level up several notches A colleague recently sent us this picture of a professional fighter who went to a surgeon for hip pain. He was told he had a labral tear based on an MRI and that his hip was degenerative because of hip dysplasia. As you know, we have grave concerns about the diagnosis of hip impingement as a large section of the population of patients without hip pain has impingement based on one study.
Aksanaku/Shutterstock
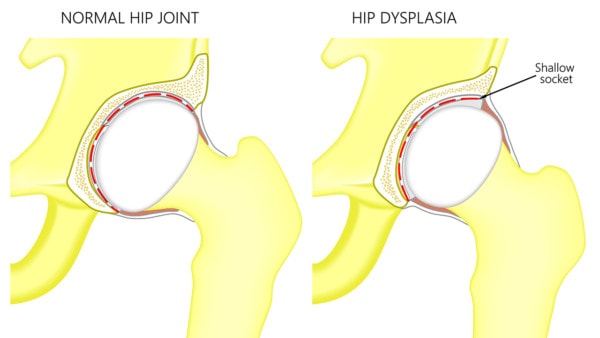
First, what is hip dysplasia? This means that the socket for the ball of the hip bone (femur) is too short or shallow. How reliable are we as doctors with measuring how severe this might be? Turns out, not very accurate according to one recent study. More concerning is a study in May of this year with the following conclusion, “Hip congruency has long been cited as a requirement for a reconstructive pelvic osteotomy, but based on the above findings, there is no clear agreement regarding what comprises a congruent joint.” Huh? So on the deciding who has hip dysplasia, we doctors can’t all agree based on these two studies.
Hip dysplasia is associated with earlier onset of hip arthritis, but one needs to be very careful with making a purely structural diagnosis. I am reminded of a similar age woman who had hip pain and was told she had dysplasia and would require a hip replacement at a young age. She really turned out to have an irritated S1 nerve in her back causing the hip pain. We treated the nerve and her pain went away, so much for predicting the cause of hip pain based on an MRI or x-ray.
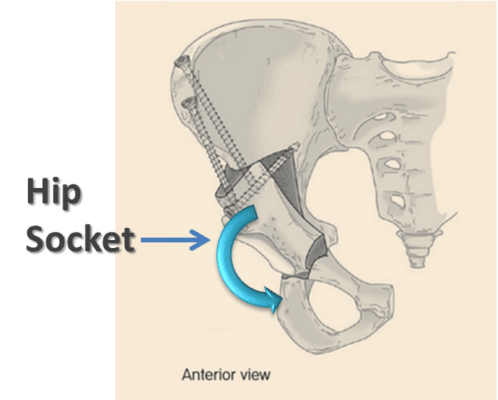
In this case, the surgeon recommended PAO surgery. This involved breaking this 33 year old active gentleman’s pelvis in 3 places on that side, so that the pelvis would be realigned and his hip wouldn’t wear anymore. You can see above the three screws off to the left of the image from moving the acetabulum (the socket of the hip). I’ve outlined in red the remaining fracture that is still there 3 months after surgery. At this juncture the structural support for the bottom of the pelvis has been severed and the gentleman can no longer lift the leg. Why? Because at this juncture his leg is only minimally attached to the rest of his body. The next step? He’s headed back for a second surgery, this time to reshape the socket through hip arthroscopy.
Where did this type of surgery originate? Similar procedures have been used to help disabled children who are non-functional for decades, and these surgeries can sometimes get them minimally more function. For young, healthy and active adults whose bones, joints, and muscles are tuned to millimeter precision, how much evidence is there that this very invasive surgery works?
First, below you’ll see a diagram of what the surgery seeks to accomplish. The entire hip socket is severed from the rest of the pelvis and turned downward to cover more of the short hip joint. So how well does this massive surgery work? Well in one recent study, 1 in 4 hips still needed a hip replacement two years later, despite the surgery. In fact, if the hip already had any type of significant arthritis (usually why patients show up to the doctor in the first place), the outcomes were worse. In 2009, a large meta-analysis (a study that reviews the results of many other studies), showed that the level of evidence supporting the procedure was the lowest grade in medicine (level 4).
How about complications from this massive surgery? In one recent Harvard study, 15% of patients had complications from the procedure. How does this compare to other procedures? Most total joint replacements have about a 7-10% complication rate.
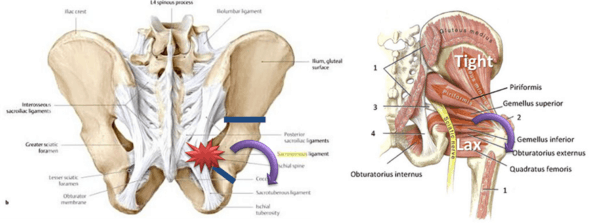
How about the other biomechanical consequences of completely restructuring the orientation of one part of the pelvis? Let’s explore this a bit because these are the patients who will show up in our clinic when they still have pain despite the surgery. Looking below there are two pictures. The one on the left is of the massive pelvic ligament complex. It predicts that the important stabilizing ligament of the tailbone (sacrospinous) will be tugged on if the hip socket is rotated downwards. The image on the right is of the muscles at the back of the hip. These muscles are fine tuned to millimeter precision in active healthy adults, so reorienting the hip socket will leave about half too loose (lax) and half too tight.
The upshot? While this massive surgery may help reduce the chance for arthritis in some patients, it’s also likely to cause other downstream bio mechanical consequences when one applies an orthopedics 2.0 assessment to the changes. Should you get this surgery? At this juncture, in my humble opinion, the jury is definitely still out.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
