Shoulder Replacement Side Effects Are Far Worse than We Thought…
Should you get a shoulder replacement? This is one of those surgeries that has a bad rap. Now new research shows why many patients complain about the results and complications of shoulder replacement.
Understanding a Shoulder Replacement
Artemida-psy/Shutterstock
The shoulder joint is an intricate ball-and-socket structure. It’s complexity in structure allows for a range of motion that is greater than any other joint in the human body. It can roll, rotate, and lift. It can move the arm straight up and down and forward and backward, and so on. No other joint is so versatile. In fact, we probably don’t realize how important the shoulder is until it becomes damaged in some way and suddenly we can’t reach up into a cabinet without pain. Because of the millimeter precision of every structure in the joint (from the nerves to the muscles, tendons, and ligaments, to the joint itself), it’s impossible to replace it and have an artificial joint function exactly like the original.
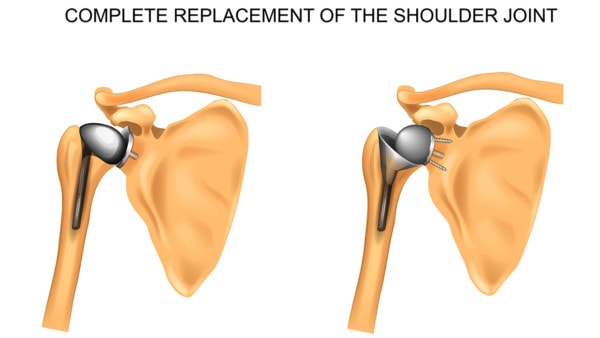
A shoulder replacement surgery involves amputating the shoulder joint. This consists of cutting through muscles and other tissues to access the joint and then removing the proximal end, or head, of the humerus (or upper arm) bone, also known as the ball. The glenoid process, or socket, of the shoulder blade is then shaved out and resurfaced. A plastic prosthetic socket is cemented into the glenoid process. The upper part of the humerus bone is hollowed out, a metal stem is inserted into the bone, and a metal head is attached to the end.
Surgically resecting the entire joint and then getting an artificial plastic and metal device to successfully pair with this complex system of structures without the nerve signals to control timing and force is incredibly challenging, and damage to these other structures is inevitable in the process, which I’ll discuss a bit. With all of these complexities to consider with a shoulder replacement, it’s probably not surprising that a new study also reveals that complications associated with the surgery are much worse than we thought. Let’s review.
Serious Shoulder Replacement Side Effects and Risks Vary Depending on Age
The new study analyzed the outcomes of over 58,000 elective shoulder replacements for arthritis over a 19-year period in Great Britan. The results? While all age groups were found to have a risk of shoulder replacement failure, men aged 59 and under fared the worst with 1 in 4 requiring revision surgery (women in the same age group were only slightly less), and the risks of revision surgery in all age groups were highest within five years post surgery. Other complications associated with the surgery included respiratory infections, UTIs, acute kidney injury, pulmonary embolism (higher in age 50-64 women), heart attack, and all-cause death (death from any cause), and these resulted in hospital admissions for 46 of every 1,000 surgeries. In these cases, older patients (particularly men age 85 and older at a rate of 1 in 5 men with 1 in 18 dying within 90 days of surgery) were most affected.
Interestingly, not only were the numbers of serious complications high in this study but the actual number of shoulder replacements performed increased each year, 5.6-fold over the 19-year period. Prior to this study, the general thought was that serious complications following shoulder replacement were uncommon, but this study found quite the opposite, and this was particularly true in younger shoulder replacement patients.
In the 85 and older group, the stress of a such a major surgery may explain the shoulder replacement side effects and some of these high complication and mortality rates. But why are younger patients experiencing shoulder replacement failures at such a high rate?
The Earth Shattering Conclusion of the New Shoulder Replacement Study
It’s not common for orthopedic surgeons to rip on their own surgeries, even in research studies, but that’s what happened here. This is what the authors of the above study concluded:
“All patients should be counselled about the risks of serious adverse events. These risks are higher than previously considered, and for some could outweigh any potential benefits. Our findings caution against unchecked expansion of shoulder replacement surgery in both younger and older patients.”
Hence, the authors of this study are questioning whether we should be offering shoulder replacement surgery to some patients. They also are concerned that the study demonstrated a dramatic expansion of the number of shoulder replacement surgeries per year.
Shoulder Replacement Failure in Younger Patients
This isn’t the first time a study has found disturbing results in younger shoulder replacement patients. A few years ago, I shared one that found even higher numbers—4 in 10—of shoulder replacement failure in the under-55 age group. In this case, revisions were necessary in these patients within the first 10 years after surgery. Imagine undergoing a second shoulder replacement before you reach 65, which would still be considered young even for the first replacement. Even without failure of the device, artificial joints are designed for older people and, as such, they aren’t designed to last forever, so the younger you get a joint replaced, the more likely you are to get it replaced again.
In addition, younger patients are simply more active than older patients. In other words a 55-year-old shoulder replacement patient will expect a lot more from his or her artificial joint than an 85-year-old patient. This means the more stress that is placed on the prosthetic shoulder, the faster it will break down. I’ve covered this issue before as it relates to knee replacements in younger patients.
The fact that a younger patient is even recommended for such an early shoulder replacement may mean that there other issues at play here that may predispose these patients to poorer outcomes, or it could create more problems in the process. For example, one study found that shoulder replacement generally damages the rotator cuff muscles in the shoulder! So, according to the study, no matter how well the shoulder device is arranged, the damaged shoulder muscles may never function normally. Abnormal forces, especially in a younger group that is likely to place more excessive forces on the shoulder, could have devastating long-term impacts on the new joint, such as early failure of the device.
Finally, the shoulder pain may not have been coming from an actual shoulder problem in the first place. It may be a result of shoulder instability due to ligament damage from either trauma or simply long-term wear and tear. A shoulder replacement isn’t going to address this problem, and the instability left unaddressed will only create more problems shoulder replacement or not. Learn more about this in my video below:
The upshot? The authors of the above study suggested that maybe it’s time to give up the practice of replacing shoulders in some patients. Why would the orthopedic surgeons who authored the study recommend this? It seems like they were blown away at the complication and surgical revision rates in this procedure.
Originally published on

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
