Shoulder Surgery Complications Caused by Acromioplasty
Shoulder decompression surgery, otherwise known as an acromioplasty, involves removing part the acromioclavicular (AC) joint structures and ligaments from the shoulder and is usually done in conjunction with a rotator cuff repair. The rational is that the bones and ligaments are impinging (pressing) upon the rotator cuff, so the surgeon performs an acromioplasty (cutting the ligaments and shaving the bones) to free up the space. On the surface it sounds logical; however, when you cut some of the major stabilizing ligaments of the shoulder, there are deeper issues beneath the surface you may have to contend with, such as shoulder instability, arthritis, and additional rotator cuff injuries.
Today, we’re going to take a live look at a moving X-ray of a patient’s unstable shoulder following an aggressive AC joint resection (the big brother of acromioplasty) and talk about the shoulder surgery complications that can result from an acromioplasty.
Where and What Is the AC Joint?
Alila Medical Media/Shutterstock
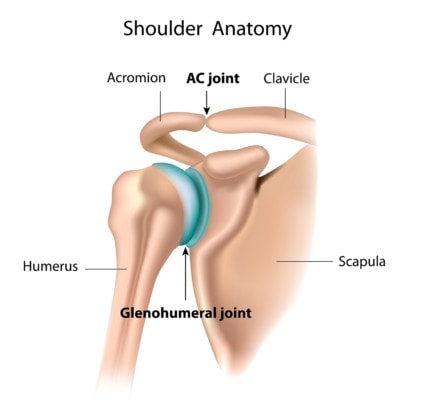
For most of us, it should be easy to locate the AC joint. Place your fingers on your collarbone (the clavicle) at the base of your neck and follow it toward your shoulder. The clavicle is straight and smooth until you come to a “speed bump” type of prominence as you reach the shoulder, almost as if it’s a warning to slow down before you reach the top curve of the shoulder. This prominence is the AC joint, and if you continue to follow the path with your fingers, just beyond the joint is the acromion bone of the shoulder—hence the name acromioclavicular joint as it bridges the clavicle (collar bone) to the acromion (front projection of the shoulder blade).
When the AC joint develops arthritis or is misshapen, it can place pressure on the rotator cuff. When this doesn’t get better with physical therapy, often surgical decompression (acromioplasty) is performed. Acromioplasty involves cutting off the bones pressing on the rotator cuff and removing important stabilizing ligaments that live there. So besides the obvious—it’s rarely a good idea to cut out something we were intended to have (as I’ve said before, the body has no spare parts)—why is acromioplasty often a bad idea?
Let’s start with the research.
What Does the Research Show Regarding Acromioplasty?
Not surprisingly, the research does not shine a positive light on acromioplasty. This past January, I shared a large randomized controlled trial showing that there is no advantage to adding an acromioplasty to a rotator cuff repair. Specifically, the study stated that findings were “consistent with previous research reports in which there was no difference in functional and quality-of-life indices for patients who had rotator cuff repair with or without acromioplasty.” In addition, the acromioplasty creates longer and more difficult recovery times for patients.
Taking this a step further, in 2014 I shared a study showing that not only rotator cuff repair with acromioplasty but also rotator cuff repair alone for rotator cuff tears due to wear and tear couldn’t outperform physical therapy.
I reported back in February that rotator cuff repair with acromioplasty is the most common shoulder procedure in the U.S., yet the study I highlighted showed that it was actually accomplishing the opposite of what surgeons thought. The purpose of the procedure is to reduce the forces on the injured rotator cuff, but the procedure actually increased them. The authors concluded that acromioplasty “increase(s) the rotator cuff force required to maintain normal glenohumeral biomechanics by 25% to 30%.” So in a bizarre twist of concept, acromioplasty doesn’t reduce forces on the shoulder rotator cuff repair—it actually makes them worse!
Let’s finish by looking at what really happens after this surgery.
A Moving X-ray of Shoulder Surgery Complications Caused by Removing the AC Joint
First, watch the short video at the top of this post to view the live, moving X-ray of one patient’s shoulder after undergoing an AC joint resection. If a picture is worth a thousand words, a moving picture is worth ten thousand. In the video, you will see the patient’s collar bone and the huge gap in the bone where the AC joint was lopped off by the surgeon. It’s that gap, you will see, that leads to these deeper problems and causes significant instability in the shoulder.
In the moving X-ray, we begin with the patient’s shoulder down and relaxed, the huge gap clearly visible. As we watch the patient’s shoulder move upward, the gap closes in. Remember, this gap is where the AC joint used to live before it was excised, where the ligaments kept the shoulder all nice and stable. This constant opening and closing of the gap means that the shoulder is grossly unstable and is beating up the shoulder with every movement. No wonder this poor guy’s shoulder pain got worse.
The upshot? As you can plainly see with you own eyes, the shoulder surgery complications created by removing the AC joint (the big brother of acromioplasty) create more problems than the surgery solves. In addition, the research doesn’t support that an acromioplasty benefits a rotator cuff repair, and, in fact, shows quite the opposite—that it makes the forces on the rotator cuff worse, not better—leading us to again ask an urgent question. Why in the world is this procedure still so commonly done? While there may be a few patients where it should be done, acromioplasty is just not a good idea in most cases. In addition, it’s a permanent bio mechanical change that can’t be undone, so once you head in this direction, nobody can give you a stable and normal shoulder back!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
