Healing Spontaneous Osteonecrosis of the Knee without Surgery
SPONK is one of those medical terms that just sounds strange, but it’s a really big nasty problem. This is the story of a patient who developed spontaneous osteonecrosis of the knee likely due to excessive knee steroid shots, who was told she needed a knee replacement, but who instead used injections of her own stem cells to solve the issue. Let’s dig in.
What Is Spontaneous Osteonecrosis of the Knee?
Osteonecrosis is a disease where a section of the bone dies off. This usually happens in the hip, but it can also happen in the knee (1). Oftentimes the disease has no known cause. However, one of the causes of osteonecrosis that is well researched is steroid use (like anti-inflammatory steroids given for pain). Abbreviations for Spontaneous Osteonecrosis of the Knee include SPONK and SONK.
The biggest long-tern problem with all osteonecrosis lesions is that they can collapse. They also destroy the cartilage in joints. Hence, they can end up causing a joint where the bone is dead, the shape of the joint has been damaged through collapse, and the cartilage is broken or gone.
How Do You Treat Spontaneous Osteonecrosis of the Knee?
The most common treatment for spontaneous osteonecrosis of the knee is either a bone decompression and graft or a knee replacement (1, 2). For a decompression surgery, the surgeon drills a tunnel into the lesion and usually adds bone graft from the patient or a cadaver. The hope here is that the bone graft takes hold and makes the area stronger.
Knee replacement is another option. This is where the existing joint is amputated and an artificial knee prosthesis is inserted. However, the osteonecrosis lesions themselves are weakened and abnormal bone which makes it harder for a knee prosthesis to bond to the bone.
The problem with both these surgeries is that they are very invasive orthopedic procedures.
Percutaneous Bone Augmentation with Orthobiologics
A longstanding alternative to surgery for osteonecrosis has been using the stem cells from the patient’s own bone marrow to help heal the dead bone. Stem cells from bone marrow can replace dead bone cells so this approach makes sense. In addition, this less invasive procedure only requires an injection of those cells to the right spot, skipping the surgery. This technique has been successfully used in other joints like the hip for decades and has been shown to heal these lesions (3).
This Patient’s Story
This is an initially tragic story of a 50-year-old woman with first knee arthritis and then knee osteonecrosis. Her problems began in May of 2019 after a knee cortisone injection. Rather than getting better, she soon became wheel-chair bound due to the pain.
One of the notable and different things in her care was that her orthopedic surgeon’s approach to her knee pain and arthritis was to perform multiple repetitive steroid shots in the knee. He reasoned that this would provide her pain relief until the knee cartilage was completely destroyed by the injections and then they would perform a knee replacement.
The irony? Steroid shots increase the risk for bone osteonecrosis, so she ended up with spontaneous osteonecrosis of the knee and not able to get a knee replacement due to the poor bone quality caused by that disease. Hence, her orthopedic’s surgeon’s approach to her knee arthritis may have placed her in a very tough place.

The patient was seen by one of our former fellows and Regenexx network provider Chris Williams, M.D. in Atlanta. Shown here is the x-ray image demonstrating Dr. Williams placing the patient’s own bone marrow stem cells mixed with a demineralized bone matrix into the osteonecrosis lesion. You can see the trocar (a specialized bone needle) here being placed into one of the lesions. No surgery is required as this is an advanced injection. At 6 weeks the patient was pain-free and began walking with some discomfort.
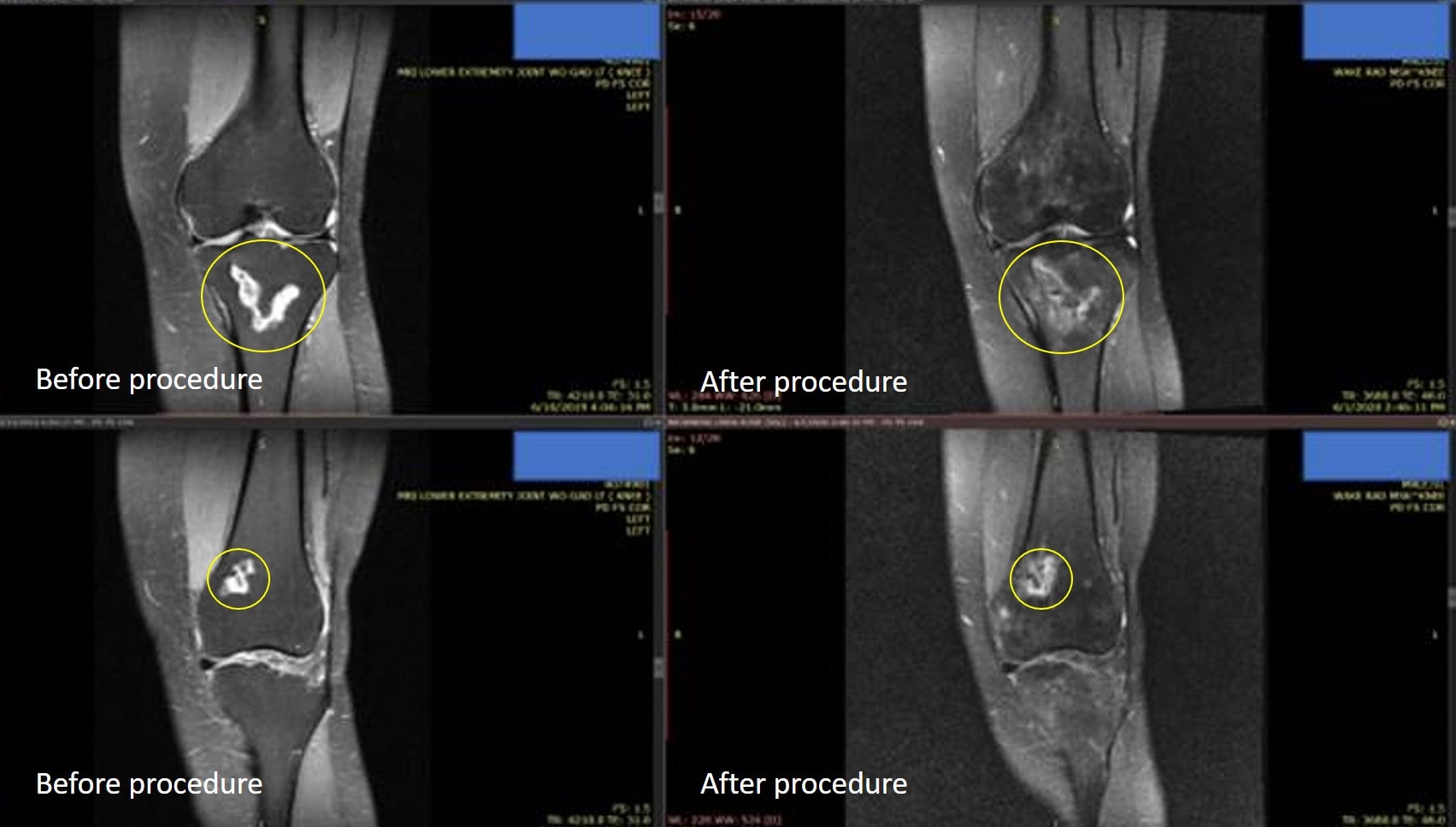
The pre and post-MRIs are below. Note that the SPONK lesion in the yellow circles shows good bone development. You can tell this because, in this image, the bright white color on the before image indicates dead bone. The darker infill on the after image indicates bone beginning to enter the lesion. After this positive finding, she was cleared to slowly return to more walking with a cane. She now no longer needs high-dose narcotics to function.
The upshot? Spontaneous osteonecrosis of the knee is a real problem that has few elegant solutions outside of invasive orthopedic procedures. However, less invasive treatments can use the stem cells from your bone marrow to prevent these lesions from collapsing. We wish this patient well on her continued recovery!
____________________________
References:
(1) Jauregui JJ, Blum CL, Sardesai N, Bennett C, Henn RF 3rd, Adib F. Unicompartmental knee arthroplasty for spontaneous osteonecrosis of the knee: A meta-analysis. J Orthop Surg (Hong Kong). 2018;26(2):2309499018770925. doi:10.1177/2309499018770925
(2) Karim AR, Cherian JJ, Jauregui JJ, Pierce T, Mont MA. Osteonecrosis of the knee: review. Ann Transl Med. 2015;3(1):6. doi:10.3978/j.issn.2305-5839.2014.11.13
(3) Hernigou P, Flouzat-Lachaniette CH, Delambre J, et al. Osteonecrosis repair with bone marrow cell therapies: state of the clinical art. Bone. 2015;70:102‐109. doi:10.1016/j.bone.2014.04.034

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
