Sub-surgical Knee ACL Instability Can Go Undetected
©Regenexx
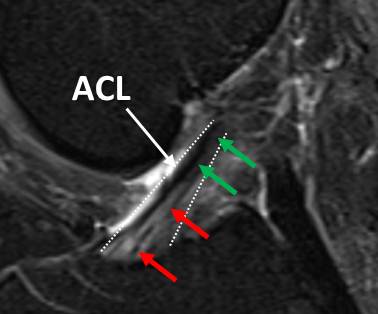
I performed an evaluation on a patient from Wisconsin this week who had a knee MRI that demonstrated a significant posterior medial knee meniscus tear and a smaller lateral meniscus tear. There was absolutely no mention of his ACL in his MRI report. One surgeon had told the patient he had a knee plica syndrome that would need surgery, a second surgeon said he would take out 50% of the medial meniscus, and finally a third surgeon told him that surgery wouldn’t help. The patient understood that taking out the meniscus would leave his knee less protected and cause more arthritis in the long run. When he was evaluated on the phone to determine his candidacy for our knee stem cell procedure, I noted his MRI did show a bright area in the ACL ligament where it anchors in the tibia. On his MRI image above, note that in this water based T2 Fat Sat image the ACL (course delineated by the dashed white lines) has normal dark signal at the top (green arrows) and brighter signal toward the bottom (red arrows). The areas marked by the red arrows aren’t at all normal and are swollen (fluid shows up as a lighter color on these knee Fat Sat MRI Images). This light area in the otherwise dark ACL ligament indicates a clear stretch injury within the ACL ligament, indicating that there is an ACL ligament problem. Despite the clear abnormality, the radiologist didn’t read this finding. The patient also reported his knee felt loose and unstable-a clear sign of instability due to a loose ligament. None of the surgeons he consulted mentioned the MRI changes nor told him his ACL was loose., nor discussed his recovery plan from this stretched ACL knee ligament. How did the knee look on examination? On exam this week in our clinic, it was obvious his ACL ligament was lax as the tibia pulled forward much more on that side. We used a device to measure the movement in his knee allowed by the ACL, which was about 4 1/2 mm on this side compared to half that amount found on testing the other knee. Again, clear signs of ACL laxity.
We see this problem in the clinic quite a bit-the lack of diagnosis of mild to moderate stretch injuries of key knee ligaments such as the ACL. Why does this important finding go unnoticed? We believe some radiologists don’t report these loose ACL ligaments because they consider this finding to be just part and parcel of an arthritic knee, so while they may see the abnormality, they don’t consider it noteworthy. We also believe many surgeons don’t comment on the ACL laxity because it isn’t enough to warrant an ACL ligament replacement surgery. Despite there not being enough laxity to require surgery, the laxity leads to significant problems such as additional swelling and arthritis in the joint. What’s the solution? If regenerative medicine treatment is considered, the ACL needs to be treated as well. In this patient, I used c-arm fluoroscopy to inject the ACL along with his ultrasound to inject the meniscus tear. In the ACL injection image below, note the darker radiographic contrast tracking up the ACL ligament (white arrows).

There is no way to accurately inject the ACL without a c-arm fluoroscope. As an example, when we use contrast dye that shows up as dark on the x-ray (as above), an inexperienced physician using x-ray guidance is actually in the ACL ligament about 1 in 10 times. It’s only once the physician learns this specific knee ACL injection technique developed by our clinic that he or she can accurately place cells in the ACL tendon sheath. In contrast, getting into this ligament blind without imaging would be a crap shoot at best, just as injecting the ligament with ultrasound would be difficult. This is because the ligament is buried in a bony tunnel (trochlear groove) and ultrasound works by bouncing sound-waves off the structure which must return to the machine to be turned into an image.
Does your knee have a loose ligament that no one has diagnosed? Does your MRI show problems within the ACL that weren’t read by the radiologist? We observe undiagnosed loose ligaments often enough for us to believe that there are many patients with loose ligaments perpetuating their knee problems who are unaware of the problem. Injecting stem cells or PRP into these joints is unlikely to help until the ligament issues are identified and specifically targeted with treatment.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
