Supraspinatus Tears & Stem Cells – Clinical Trial Returns Jiu Jitsu Competitor to the Podium
This is a guest post from Regenexx® Dr. Jamil Bashir from the Centeno Schultz Clinic in Broomfield, Colorado
Creating a new field of Medicine is no easy task. Change always encounters resistance and transforming thought cannot occur without evidence, reproducible evidence. In Medicine, clinical trials are the standard used to produce such evidence.
With the intention of evaluating the efficacy of the revolutionary procedures offered by Regenexx clinics throughout the country, the task of developing clinical trials began a few years ago. Multiple clinical trials are currently underway, with the aim of critically examining our own techniques and sharing the outcomes with the scientific community. One of these trials is aimed at evaluating the success of Bone Marrow Concentrate (of which adult Mesenchymal cells are a part) injections directly into Supraspinatus Tendon rotator cuff tears.
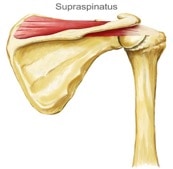
Supraspinatus muscles extending from it’s origin atop the scapula in the supraspinatus fossa, to it’s insertion onto the Greater Tubercle of the Humerus.
The Supraspinatus is one of four muscles that compose the musculature that gives motion to the shoulder, collectively termed the rotator cuff. It has its origin (starting point) on the top on the scapula and extends laterally to insert (endpoint) onto a prominence on the humerus termed the greater tuberosity. Like all muscles, the muscle morphs into a tendon as it attaches to its insertion site on the bone (in this case the humerus). This transition point between muscle and bone is termed an “enthesis.” Think of your body as a skeleton, a framework of bones resisting the constant downward force of gravity. To get your skeleton to move, muscles must contract (shorten in length) thereby bringing the bones they bridge closer together. This is how movement is generated.
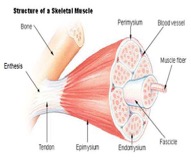
Schematic drawing of the components of the muscle/tendon complex showing the enthesis attachment at the bone surface.
Developing this clinical trial involved all the normal tasks in such an endeavor. Careful criteria must be described and patients must be sure to fit into these inclusion criteria to be entered into the study. For example, the rotator cuff is actually composed of four muscles with their associated tendons, Supraspinatus, Infraspinatus, Subscapularis and Teres Minor. In order to reduce variables that could cloud the outcome of the study, patients had to be screened to ensure that only the Supraspinatus, and none of the other rotator cuff muscles (or other parts of the shoulder) were damaged.
One such candidate for the study was JS, a Brazilian Jiu Jitsu practitioner, who visited our clinic by way of Las Vegas. JS is a very personable 28-year-old gentleman who had torn his Supraspinatus muscle while weightlifting one-year prior and had read about the work we are doing here at Regenexx. From his own description, the use of the body’s own healing cells to produce tissue repair deeply resonated with him. He had heard of our clinical trial and had set up an appointment for an evaluation. Upon review of his MRI and through a careful physical examination as well as Ultrasound study, we determined he would be a suitable candidate for the study.
At this point he was triaged into either a treatment group that received treatment immediately, or a control group, that would undergo 6 months of Physical Therapy. The purpose of a control group in clinical trials is to establish a way of comparing the treatment group with a second group that does not undergo the treatment and instead partakes in another conventional modality, in this case Physical Therapy. This allows the researcher to eliminate the possibility that a successful outcome from the treatment group is not just a function of natural healing that would have taken place over time of its own accord.
Supraspinatus Tendon Tear Treatment with Precise Stem Cell Injections
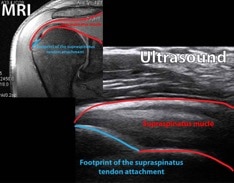
Imaging revealing correlation of MRI imaging to Ultrasound findings.
JS was triaged to the treatment group and underwent a bone marrow draw and re-injection into this Supraspinatus tendon under Ultrasound guidance, with careful correlation of the Ultrasound imaging to his MRI imaging to maximize the efficacy of the procedure.
Our procedures are carried out meticulously. Long training and study enables us to not only accurately visualize injuries but also to apply the correct techniques to maximize repair. For instance, if you recall earlier the transition point termed the “enthesis” site is where muscle morphs into bones. This area is actually rich in osteogenic (bone generating) stem cells. Through careful agitation with the tip of our needle after appropriate local anesthesia is provided, we are able to stimulate the local bone stem cells present in the superficial periosteum to transform into enthesis tissue thereby anchoring the stem cells placed into the tendon and muscle belly to the bone. These and other long researched techniques enable us at Regenexx to continue to push the envelope of Regenerative Medicine.
The placement of the stem cells and other progenitor cells directly into the muscle allows the cells to begin to act on local cells within the tissue and begin repair, as well as to begin to differentiate into new target tissue themselves. Mesenchymal stem cells (MSCs) are termed such because they derive from the Mesoderm of the early embryo. When life is beginning to develop, all cells are similar, then quickly three cell lines develop in the early embryo termed the mesoderm, endoderm and ectoderm, Classically, endoderm gives rise to organs, ectoderm to nerves and skin, and mesoderm to connective tissue (bones, tendons, ligaments, cartilage, muscle, blood vessels everything we work to heal here in the field of interventional orthopedics / regenerative medicine). This is the difference between embryonic stem cells and adult MSCs. The embryonic stem cells are capable of becoming any cells from any of the three early cell lines as they represent the earliest cells before the split into the three lines. The adult mesoderm cells (MSCs) can “readily” only become connective tissue–And I say “readily” because in 2012 a Japanese and English research pair won the Nobel prize by proving that even adult cells under the right condition could revert back to embryonic cells and thus give rise to all three lines, thus turning the scientific world on its head and humbling all to the realization that there is still much to learn [see link for more details: http://www.nobelprize.org/nobel_prizes/medicine/laureates/2012/press.html].
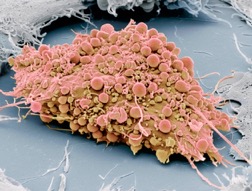
Scanning Electron Microscope of an Adult Mesenchymal Stem Cell showing the surface cell processes and receptors
MSCs differentiate (transform) into different types of tissue by a number of theories. One of which is cell contact. If you see a cell under an electron-scanning microscope it has tentacles or processes that allow it to attach to local tissue.
Once attached, surface proteins specific to the target tissue bind to receptors on the MSCs surface, transmitting messages into the nucleus where DNA is housed. These messages tell the DNA which genes should be expressed to generate new cells to replace the damaged tissue that the MSC have recently come in to contact with. Our bodies are truly brilliant, and intricately simple.
Once placed, the cells need direction. It is like placing the worlds greatest reconstruction team directly into a damaged area, they will perform at their best with proper direction. One way of stimulating the cells and optimize their growth is through exercise. The use of proper rehabilitation exercises after our procedures such as eccentric (the negative of a lift) allows the cells to gain mechanical stimulation in the correct fashion and facilitate proper growth. Long known to be one of the most effective ways of generating muscle and tendon repair (eccentric exercises in and of themselves actually act on local stem cells in the muscle to direct differentiation of injured tissue), the use of eccentric exercises (resistance against the muscle as it is lengthening as opposed to contracting or shortening) over the course of a few weeks enabled JS to optimize his recent stem cell based procedure.
A Return to the Podium Following Non-Surgical Supraspinatus Tear Treatment

Photo of medal presentation at JS’s Jiu Jitsu tournament (JS is to the right)
Five months after his treatment, JS, reported full return of range of motion and strength and was cleared by our clinic to return to competitive Jiu Jitsu. A few months later he took third place in a Jiu Jitsu competition and through his successful healing process, and friendly nature, helped to inspire those of us engaged in creating the new field of Regenerative Medicine to boldly forge ahead.
There is an art to healing, and unfortunately as needed as clinical trials are to advancing the credibility of this new field, they are by their nature inherently lacking. For instance, if you have had the opportunity to read Dr. Centeno’s informative book – Orthopedics 2.0, you have heard the idea that everything is connected (and if you haven’t, I encourage you to download the free e-book and empower yourself by learning the workings of your own body). Problems upstream and downstream from an injury can affect the recovery and very well may have been the causative factor. To demonstrate the limitations of clinical trials, imagine a patient with a severely herniated cervical disc that impairs the electrical output from its associated spinal nerves. For the rotator cuff, the 5th and 6th cervical nerve that exit from the C4-C5 and C5- C6 interspace respectively act to provide input and stimulation to the muscles of the rotator cuff. What would happen if a patient whose Supraspinatus tendon was actually caused in large part to chronic poor signaling from those nerves that made the muscle susceptible to damage? Without treating the associated nerves and improving the electrical input, the muscles’ ability to heal would be limited despite the injection of your body’s own very potent bone marrow derived MSCs.
Herein lies the art of medicine, knowing that our patients are people and people are unique. They are not subjects to be divided into study and control groups as a statistic, but need to be assessed individually as no two injuries or people will ever be exactly the same and each requires an astute clinician to ascertain how best to provide for that patient. Things being what they are, however, we are working hard to produce clinical trials that fit into the limited medical paradigm that we are operating in. Somehow we must help patients, and the medical community as a whole, become aware that the knowledge of how the body heals itself is rapidly coming to light; thereby, potentially offering higher levels of healing at lower costs, which will be good for us all.
* For references please email [email protected]

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
