The BEAR Implant for ACL Tears

Credit: Shutterstock
ACL reconstruction surgery has been a staple of modern sports medicine for decades. However, now a new surgical implant called BEAR is shaking up that world by offering a solution to try to “regrow” the torn ACL. Let’s look at the positives and negatives of this new technology and compare it to the Regenexx perc-ACLR procedure.
ACL Reconstruction Surgery
When a patient tears the Anterior Cruciate Ligament (ACL) in the knee and physical therapy cannot return that individual to sports, ACL reconstruction surgery (ACLR) is usually the next step. A piece of hamstring or quadriceps tendon is harvested, and then graft tunnels are drilled into the femur and tibia. That tendon is secured in the tunnels and now serves as a replacement ligament.
The surgery, however, is not without its problems. These are:
- Only a single bundle repair of a double bundle ligament means the knee is left rotationally less stable (10)
- The graft tendon goes in at a steeper angle than the original ACL; hence it’s more likely to shear and fail (9)
- No working position sensors in the tendon repair of a ligament mean less position sense (6-8)
- High likelihood of developing arthritis/doesn’t prevent arthritis (11,12)
- Higher chance of tearing the ACL on the other knee (13)
- The hamstrings or quadriceps muscles become weaker due to the graft harvest (14)
What is BEAR?
The acronym BEAR stands for Bridge Enhanced ACL Repair. This is a bovine collagen implant inserted in the torn area of the ACL with sutures placed in graft tunnels. The BEAR implant is then injected with autologous whole blood. This allows for ACL repair.
How is BEAR different than ACLR surgery? First, BEAR allows the ACL to repair itself rather than ripping out the ACL remnants and placing a tendon as a substitute. Second, the BEAR treated ACL position is more natural than the result of ACLR surgery. Third, while it’s unknown if knees repaired with BEAR retain their position sense, that’s much more likely than the tendon graft placed by ACLR surgery. Fourth, there is no need to take a tendon graft with BEAR, so things like hamstrings and quadriceps weakness are avoided. Finally, the research on BEAR has shown a lower likelihood of tearing the ACL in the opposite knee, likely because the natural biomechanics are likely better preserved than ACLR surgery.
In a recently published Randomized Controlled Trial (RCT), the BEAR procedure was shown to be as good or better than ACL reconstruction surgery (1).
What is the Regenexx Perc-ACLR Procedure?
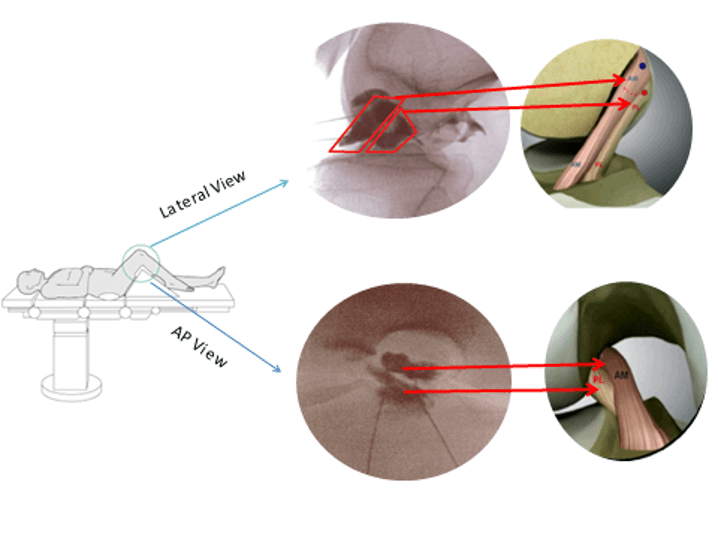
What if you could skip the surgery and instead have your Bone Marrow Concentrate (BMC), which contains healing stem cells, injected into your ACL? That’s the Regenexx Perc-ACLR procedure (Percutaneous ACL Repair). To make that happen, the doctor precisely seeds your damaged ACL with BMC using x-ray guidance (fluoroscopy). No surgery, drilling, or graft tunnels are required. To learn more, see my video below:
Our research has shown that for the right type of tears, you end up with MRI and functional evidence of a repaired ACL. Meaning these patients return to sports just like those who get ACLR surgery. The advantages are:
- A much less invasive procedure than surgery
- A normally placed ACL
- Retained position sense in the knee
- Likely lowered prevalence of early arthritis and tearing the opposite ACL as the normal biomechanics of the knee are preserved.
In past decade, we have published two MRI analysis case series demonstrating good healing of the ACL with the Perc-ACLR procedure (16,17). We published the first half of a Randomized Controlled Trial last year and have completed that trial, with the full study to be published this year (15). The results were excellent (more on those below).
Comparing BEAR to Regenexx Perc-ACLR
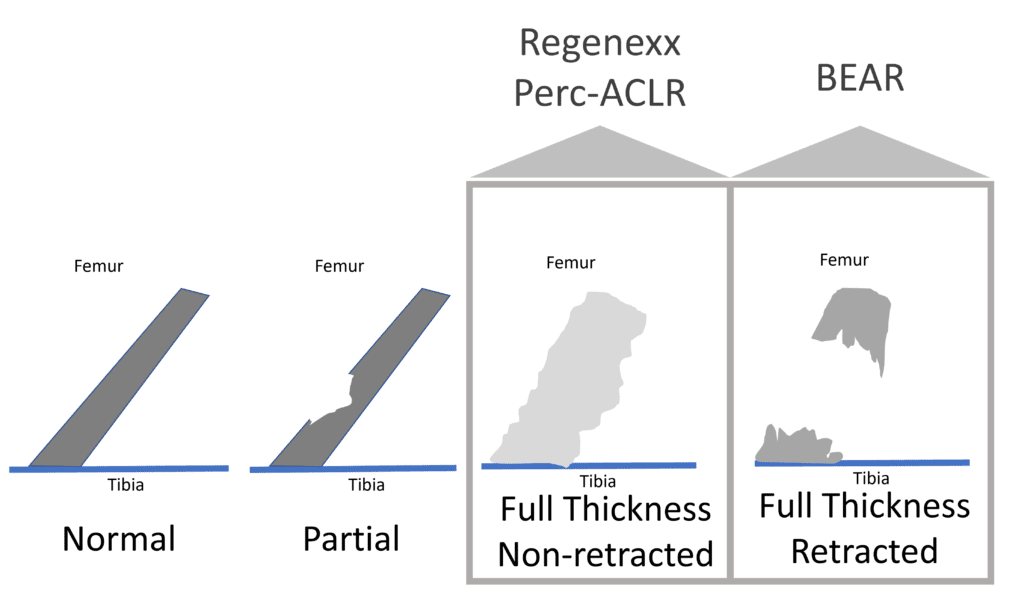
Assuming that orthopedic surgeons apply BEAR to the correct patients, these two procedures should never really compete head to head. Why? BEAR should be applied in patients with complete retracted tears, which means that the two ends of the torn ACL don’t connect and have pulled back like a rubber band. The Regenexx perc-ACLR procedure should be applied in patients that have a complete ACL tear, but the two ends are still connected. In my experience, about 1/3 of all complete ACL tears are retracted (BEAR candidate), and about 2/3rds are non-retracted (Regenexx Perc-ACLR candidate).
How can you tell which type of complete ACL tear is which? That may be tough to do using an MRI report, as the reading radiologist often doesn’t differentiate between the two tear types. Hence, you would need a Regenexx network physician to look at your actual MRI images.
However, I am concerned that orthopedic surgeons may begin to take full-thickness non-retracted tears and shove those inappropriately into the BEAR category. That would be a shame, as it’s exposing the patient to more risk than is required to get good clinical results.
Some BEAR Caveats
The BEAR Implant is Still Big Surgery
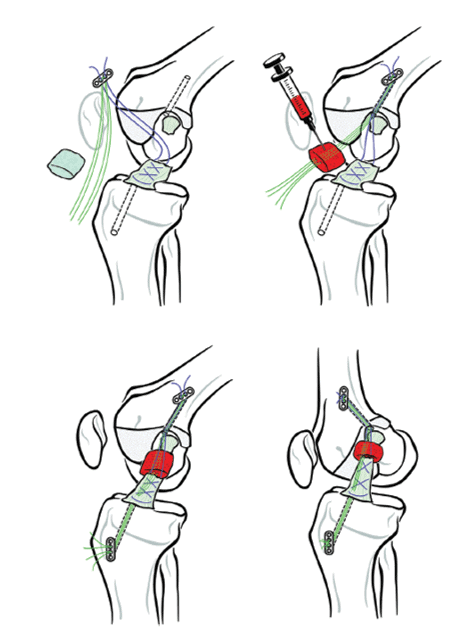
When I first heard about the BEAR ACL implant, I believed that the surgeon would place it in the correct spot and perhaps tack it down, meaning a far less invasive procedure than drilling graft tunnels. However, as shown above, just like an ACL reconstruction, the BEAR implant surgery still has the physician drill tunnels. Why is that an issue?
The problem is that the recent research from Harvard shows that drilling these graft tunnels likely means a significant second severe inflammatory hit to the cartilage (2-4). Meaning the cartilage destruction markers after an ACL reconstruction surgery are similar to those seen right after the original injury, causing a double hit to the cartilage. Hence, any implant procedure requiring tunnels to be drilled will likely harm cartilage.
Conversion to ACLR Despite the BEAR Implant
How many patients fail the BEAR implant and still need ACL reconstruction surgery? The recent trial results showed that 14% of patients required ACLR surgery despite the BEAR surgery (1). At the same time point, the Regenexx Perc-ACLR procedure had an 8% surgery rate, which more similar to the 6% conversion to a second surgery after ACLR surgery reported in the BEAR study.
Single vs. Double Bundle Repair
The BEAR implant goes into single graft tunnels drilled into the femur and tibia like ACLR surgery. This is a potential problem as the natural ACL has two bands that cross each other (hence the name “Cruciate,” which in Latin means “cross”). This double-bundle design ensures that the ACL can control the rotation of the tibia, an essential function in protecting the knee. Like the ACLR surgery, the BEAR implant only focuses on repairing a single bundle, so the knee is more likely to remain rotationally unstable.
Return to Play
Perhaps the single biggest question from an athlete is, “When can I return to play?” For ACL surgery, the current recommendations are 1-2 years. Based on what I have observed for MRI evidence of healing on the images shared by the company that makes the BEAR implant and physicians online trying this procedure, the ligament reconstitution is not complete until 12 months. Having said that, at least one study reported a higher percentage of patients in the BEAR surgery group who were more psychologically ready to return to sports at six months versus ACLR surgery (5). However, given that BEAR is a new technology, most surgeons are unlikely to allow a return to sports at six months.
Regenexx Perc-ACLR has been performed since 2012. During that time, we have observed that younger patients are ready to return to sports at four months, with older patients at six months. This quicker return to play likely represents a less severe tear type for Perc-ACLR and the use of more powerful bone marrow concentrate versus whole blood for BEAR.
Comparing BEAR to Regenexx Perc-ACLR-Summary
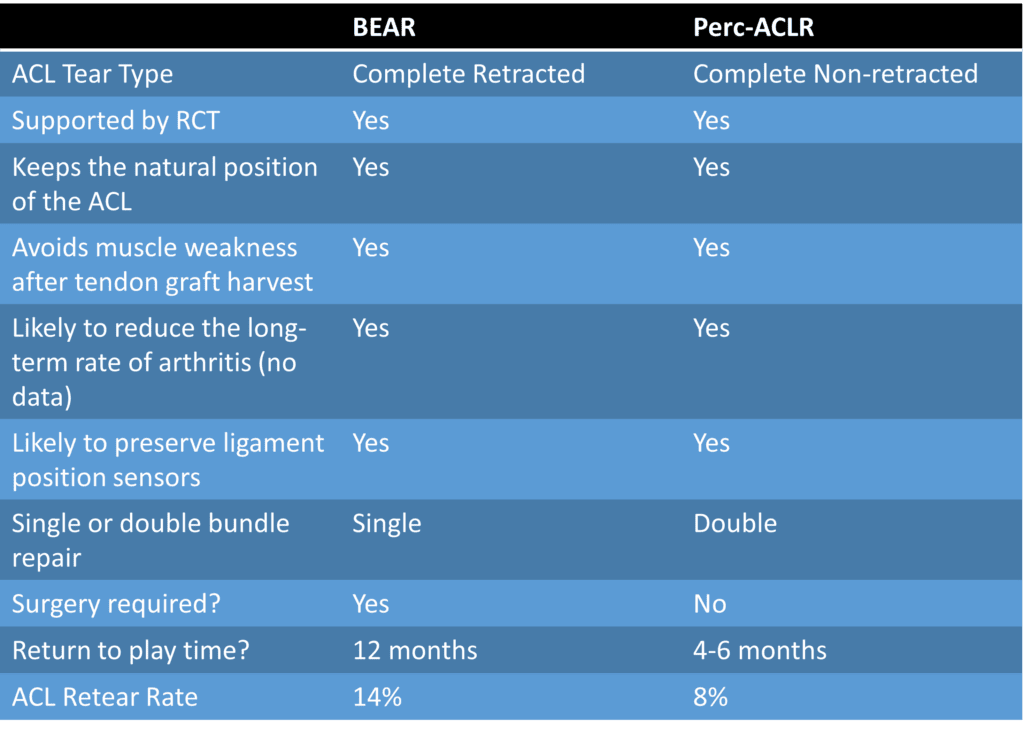
I’ve summarized the comparison above. The most significant differences are that BEAR still requires surgery, and the Regenexx Perc-ACLR procedure is a precise image-guided injection. In addition, the retear rate that we’re about to publish is lower for Perc-ACLR than BEAR, and most of our patients end up with a natural double-bundle repair which is less likely with BEAR. Finally, returning to play is likely much quicker for a precise image-guided injection than the BEAR surgery.
The upshot? BEAR and the Regenexx Perc-ACLR procedure are better than an ACLR surgery in many ways. When applied correctly to suitable patients, these two really shouldn’t compete head to head in that they are focused on two different types of ACL injuries. So hopefully, we’ll see more ACL repair than tendon grafts in the near future!
________________________________________________________________
References:
(1) Murray MM, Fleming BC, Badger GJ; BEAR Trial Team, Freiberger C, Henderson R, Barnett S, Kiapour A, Ecklund K, Proffen B, Sant N, Kramer DE, Micheli LJ, Yen YM. Bridge-Enhanced Anterior Cruciate Ligament Repair Is Not Inferior to Autograft Anterior Cruciate Ligament Reconstruction at 2 Years: Results of a Prospective Randomized Clinical Trial. Am J Sports Med. 2020 May;48(6):1305-1315. doi: 10.1177/0363546520913532. Epub 2020 Apr 16. PMID: 32298131; PMCID: PMC7227128.
(2) Culvenor AG, Eckstein F, Wirth W, Lohmander LS, Frobell R. Loss of patellofemoral cartilage thickness over 5 years following ACL injury depends on the initial treatment strategy: results from the KANON trial. Br J Sports Med. 2019 Sep;53(18):1168-1173. doi: 10.1136/bjsports-2018-100167. Epub 2019 Feb 8. PMID: 30737199.
(3) Hunt ER, Jacobs CA, Conley CE, Ireland ML, Johnson DL, Lattermann C. Anterior cruciate ligament reconstruction reinitiates an inflammatory and chondrodegenerative process in the knee joint. J Orthop Res. 2021 Jun;39(6):1281-1288. doi: 10.1002/jor.24783. Epub 2020 Jun 29. PMID: 32558951.
(4) King JD, Rowland G, Villasante Tezanos AG, Warwick J, Kraus VB, Lattermann C, Jacobs CA. Joint Fluid Proteome after Anterior Cruciate Ligament Rupture Reflects an Acute Posttraumatic Inflammatory and Chondrodegenerative State. Cartilage. 2020 Jul;11(3):329-337. doi: 10.1177/1947603518790009. Epub 2018 Jul 22. PMID: 30033738; PMCID: PMC7298591.
(5) Sanborn RM, Badger GJ, Proffen B, et al. Psychological Readiness to Return to Sport at 6 Months Is Higher After Bridge-Enhanced ACL Restoration Than Autograft ACL Reconstruction: Results of a Prospective Randomized Clinical Trial. Orthopaedic Journal of Sports Medicine. February 2022. doi:10.1177/23259671211070542
(6) Patterson MR, Delahunt E. A diagonal landing task to assess dynamic postural stability in ACL reconstructed females. Knee. 2013 Dec;20(6):532-6. doi: 10.1016/j.knee.2013.07.008. Epub 2013 Aug 18. PMID: 23962647.
(7) Bączkowicz D, Skomudek A. Assessment of neuromuscular control in patients after anterior cruciate ligament reconstruction. Ortop Traumatol Rehabil. 2013 Jun 28;15(3):205-14. doi: 10.5604/15093492.1058410. PMID: 23897997.
(8) Nyland J, Klein S, Caborn DN. Lower extremity compensatory neuromuscular and biomechanical adaptations 2 to 11 years after anterior cruciate ligament reconstruction. Arthroscopy. 2010 Sep;26(9):1212-25. doi: 10.1016/j.arthro.2010.01.003. Epub 2010 Jun 16. PMID: 20810079.
(9) Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013 Aug;41(8):1808-12. doi: 10.1177/0363546513493896. Epub 2013 Jun 28. PMID: 23813800.
(10) Song EK, Seon JK, Yim JH, Woo SH, Seo HY, Lee KB. Progression of osteoarthritis after double- and single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2013 Oct;41(10):2340-6. doi: 10.1177/0363546513498998. Epub 2013 Aug 19. PMID: 23959965.
(11) Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049-1057. doi:10.1177/0363546514526139
(12) Wirth W, Eckstein F, Culvenor AG, Hudelmaier MI, Stefan Lohmander L, Frobell RB. Early anterior cruciate ligament reconstruction does not affect 5 year change in knee cartilage thickness: secondary analysis of a randomized clinical trial. Osteoarthritis Cartilage. 2021 Apr;29(4):518-526. doi: 10.1016/j.joca.2021.01.004. Epub 2021 Feb 4. PMID: 33549723.
(13) Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42(7):1567-1573. doi:10.1177/0363546514530088
(14) Nomura Y, Kuramochi R, Fukubayashi T. Evaluation of hamstring muscle strength and morphology after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2015 Jun;25(3):301-7. doi: 10.1111/sms.12205. Epub 2014 Mar 20. PMID: 24646218.
(15) Centeno C, Lucas M, Stemoer I, Dodson E. IMAGE-GUIDED INJECTION OF ANTERIOR CRUCIATE LIGAMENT TEARS WITH AUTOLOGOUS BONE MARROW CONCENTRATE AND PLATELETS: MIDTERM ANALYSIS FROM A RANDOMIZED CONTROLLED TRIAL. Bio Ortho J Vol 3(1):e29–e39; October 5, 2021.
(16) Centeno C, Markle J, Dodson E, Stemper I, Williams C, Hyzy M, Ichim T, Freeman M. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018 Sep 3;16(1):246. doi: 10.1186/s12967-018-1623-3. PMID: 30176875; PMCID: PMC6122476.
(17) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015 Jul 31;8:437-47. doi: 10.2147/JPR.S86244. PMID: 26261424; PMCID: PMC4527573.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
