The Curious Case of the Bad Artificial Disc
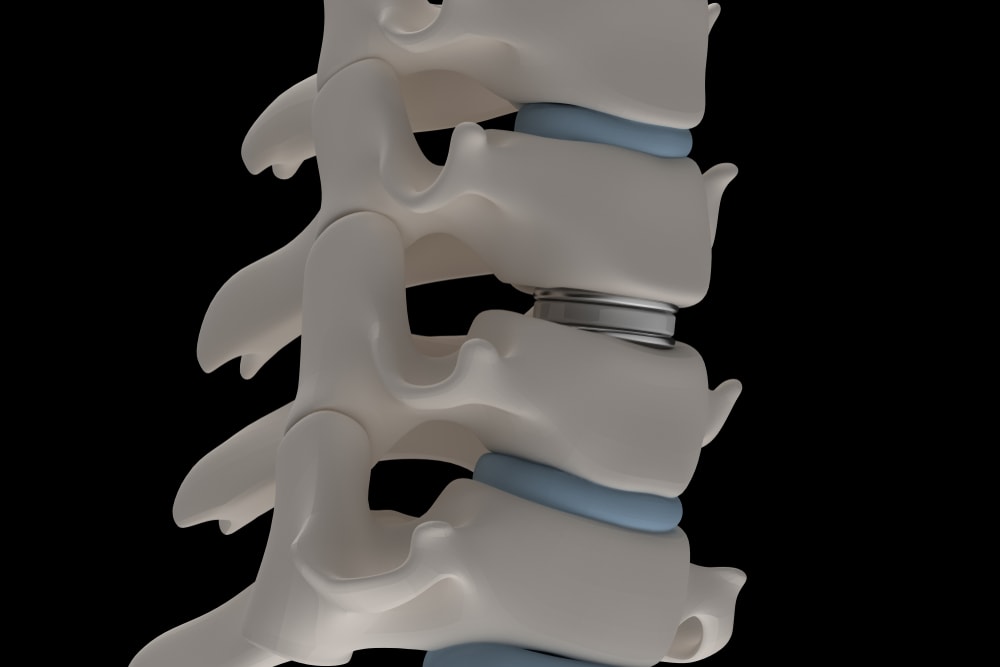
Credit: Shutterstock
I often write about what I experience day in and day out in the clinic. The case this morning is of a patient who had an Artificial Disc placed and developed new pain. After a few in-clinic x-rays, a problem with the disc was discovered. So let’s use this opportunity to review the concept of an Artificial Disc and why it’s often not as good as advertised. Let’s dig in.
What Is An Artificial Disc?
Artificial Discs were invented as a way to fix the main issue with spinal fusion. The problem is that once you bolt two parts of the normally movable spine together, you lose motion and begin overloading the adjacent levels. One way to fix that is to design a device that would take the place of the disc and allow normal motion. As a concept, this is pure genius. However, sometimes in life the idea and the execution depart from one another.
For example, ASD (Adjacent Segment Disease) is when that overload of the nearby spinal segments due to Fusion causes those levels to begin to break down. Hence, if we use ADR (Artificial Disc Replacement also known as TDR or Total Disc Replacement) and avoid a Fusion, this problem should go away. However, the research is not so supportive that this really happens.
For example, one recent study showed that after 5 years, only 38% of Artificial Discs still moved as they were designed (1). Another study showed that a third of patients needed the surgery to be repeated by 10 years after surgery (2). Yet another study showed that once you backed out the hardware removal surgeries in Fusion patients, there was no difference in the number of additional surgeries needed between an Artificial Disc and Fusion (3). Meaning, the data concerning installing a small hockey puck sized device to replace your bad disc isn’t as promising as many surgeons advertise.
My Patient
My patient is a middle-aged male who had an Artificial Disc placed at L5-S1 and a fusion at L4-L5. The Fusion was performed because he had Spondylolisthesis (a slipped vertebra) at L4-L5. So this begins as an interesting patient because he has both a Fusion AND an Artificial disc. The surgery was done at a famous back surgery site and he paid out of pocket to get the ADR as his insurance carrier refused to cover it.
His back pain was initially left-sided and the surgery helped that issue. However, he has had mounting pain since the surgical procedure now on the opposite right side. When he went back to the surgeon, the new plan seems to be to fuse the next segment up, which is L3-L4. However, there was a relatively normal discogram performed at that level plus his exam is negative there. Where his exam did show problems is at the right L5-S1 Facet joint and the SI joint.
The ProDisc-L
This patient was at this end of the day and one of our Rad Techs was walking out the door, but I convinced her to stay to get a quick shot of the ADR. After all, we needed to see whether the device was placed correctly and was still functioning as designed. To understand these x-rays you’ll need to learn a few things about ADR devices.
This is the device that was placed into my patient:
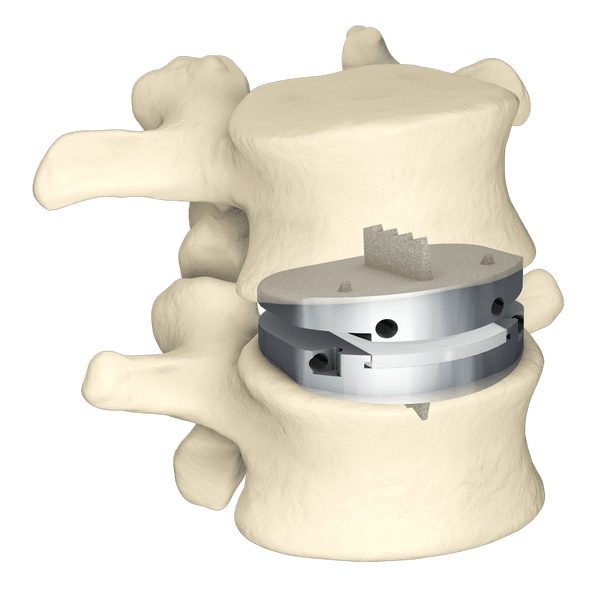
This is called the ProDisc-L made by Centinel Spine. Note how it’s made:
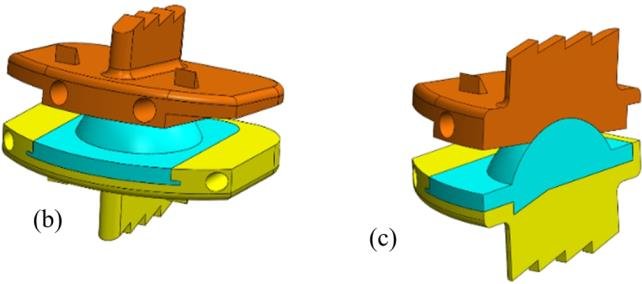
Basically, it has two plates that anchor into the vertebra with the fins that you see, and then there is a shallow cup-shaped plastic joint that allows the disc to pivot. Hence, if you bend forward or backward, the device should pivot around that shallow ball and socket.
The X-rays
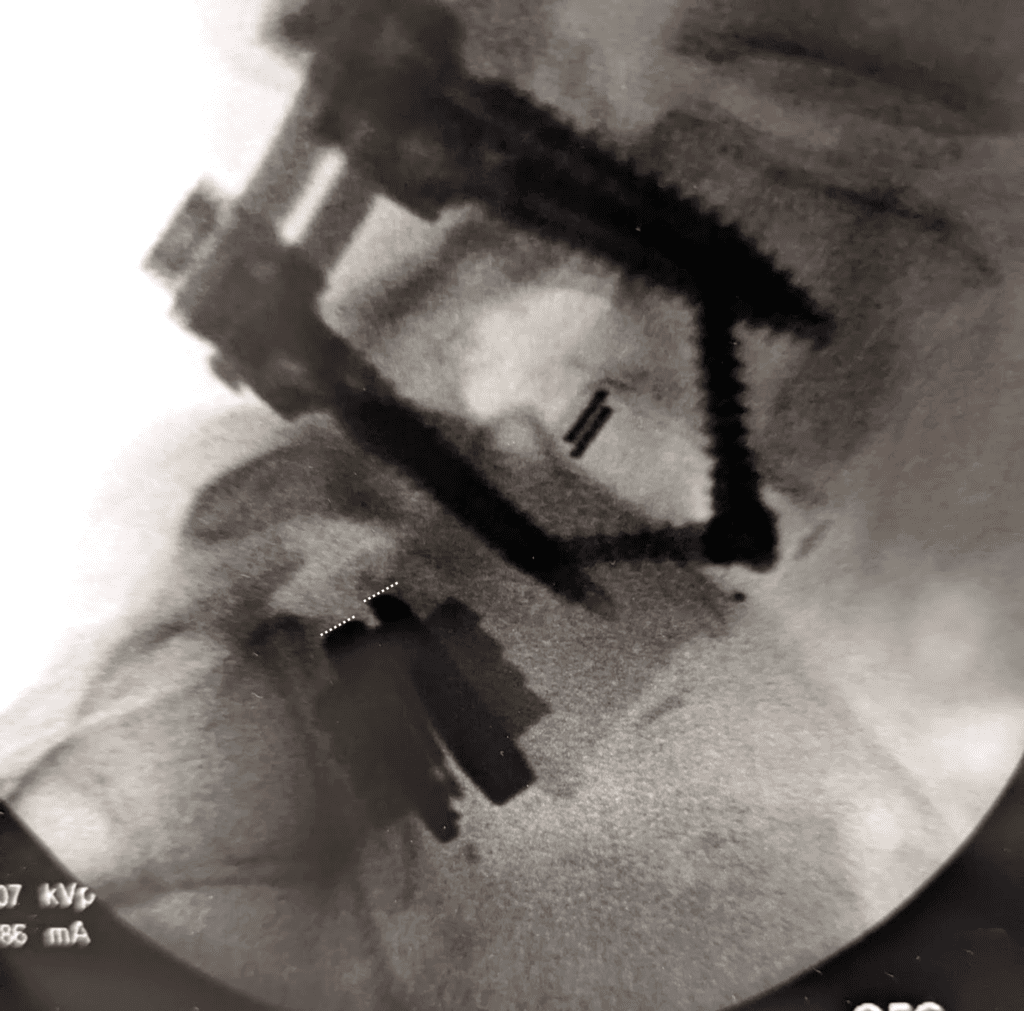
The first x-ray showed me what we were dealing with in this patient:
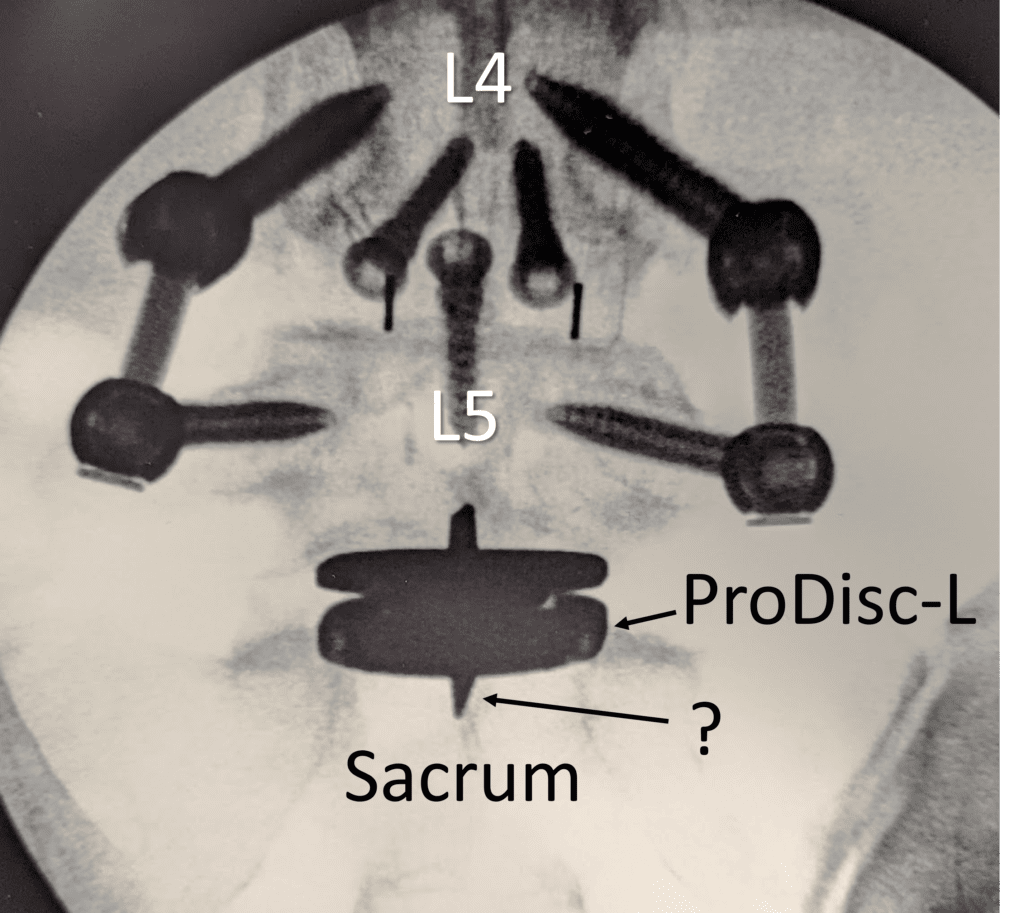
You see the ProDisc-L device. The two spike-looking things that travel up and down from the horizontal plates are actually those fins seen on edge. Notice that the one on the bottom looks bent to the left (denoted by the question mark). Could that be why my patient has new pain on the right? Maybe.
I was curious to see how this device performed with movement as while my patient has pain with standing extension, which would be normal for a Facet problem, he also has as much or more pain with flexion. Here’s the neutral lateral view:
You see the ProDisc-L below the Fusion and I have drawn two white dashed lines at the back of that device that indicate the position of the plates relative to one another. In flexion, we should see the open part between the plates in the front close and the plates rotate due to that shallow ball and socket joint. However, here’s what we actually see in lumbar flexion:
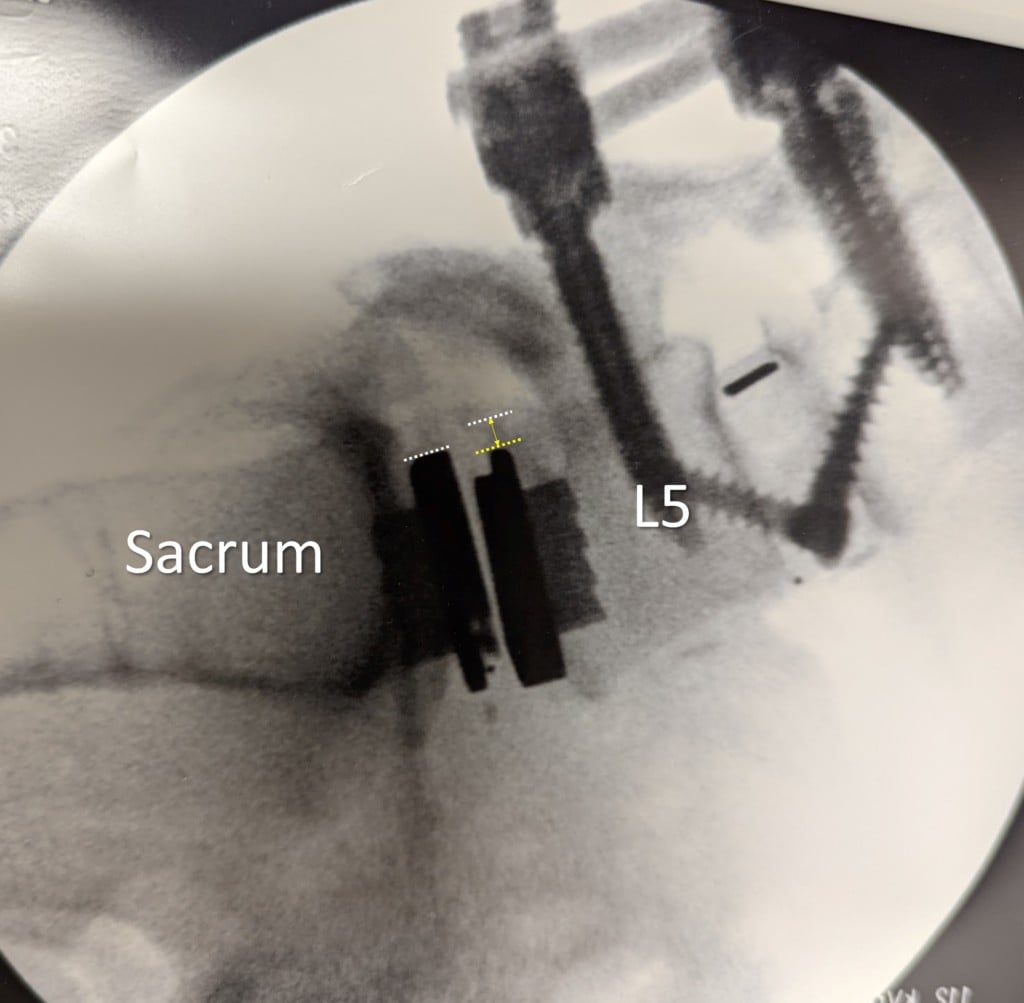
Huh? The white lines at the back of the devices now show that the L5 plate has slid forward (yellow dashed line) from its original position (white dashed line). The yellow double arrow shows the distance of the side. Why is this a big deal?
Iatrogenic Spondylolisthesis
Iatrogenic is a strange medical word that means that the doctor caused a problem. In this case, something called Spondylolisthesis which means a slipped spine. You see, the spinal vertebrae are built to rotate one on the other. However, when they slip or slide against one another, the Facet joints in the back of the spine get beat up. Here this is caused by one-half of the joint (the top L5 part) getting dragged into the bottom sacral part. So it’s no secret why this guy now has new issues at the L5-S1 Facet joints. IMHO both L4-L5 and L5-S1 segments are overloading the Facets and the SI joint below plus he has a new Spondylolisthesis created by the artificial disc.
The Solution?
The surgeon’s solution was to either fuse L3-L4 (which will make the forces here at L5-S1 worse) or to perform a Rhizotomy of the painful Facets. Given that burning the nerves that take the pain from the joint will destroy the Multifidus muscle that stabilizes this level, that will also make things worse. Our solution is to treat the Facets with orthobiologics to help them hang in there and do the same with the overloaded SI joint as well as tighten down ligaments through precise injection to add to the stability of this level. That’s while he figures out with second opinion surgeons how to fix this new issue.
The upshot? I have been very unimpressed with Artificial Discs. They seem to have a high failure rate and many times I see devices that are damaged or not working at all. In addition, I’m not convinced that the research shows that they function any better than a Fusion. In addition, when problems like this occur, you’re left with the prospect of taking out the hockey puck (ADR device) and putting in a new one, which is a BIGGER problem than the original pathology.
____________________________________________
References:
(1) Kitzen J, Vercoulen TFG, Schotanus MGM, van Kuijk SMJ, Kort NP, van Rhijn LW, Willems PCPH. Long-Term Residual-Mobility and Adjacent Segment Disease After Total Lumbar Disc Replacement. Global Spine J. 2021 Sep;11(7):1032-1039. doi: 10.1177/2192568220935813. Epub 2020 Jul 2. PMID: 32677523; PMCID: PMC8351064.
(2) Laugesen LA, Paulsen RT, Carreon L, Ernst C, Andersen MØ. Patient-reported Outcomes and Revision Rates at a Mean Follow-up of 10 Years After Lumbar Total Disc Replacement. Spine (Phila Pa 1976). 2017 Nov 1;42(21):1657-1663. doi: 10.1097/BRS.0000000000002174. PMID: 28368983.
(3) Radcliff K, Spivak J, Darden B 2nd, Janssen M, Bernard T, Zigler J. Five-Year Reoperation Rates of 2-Level Lumbar Total Disk Replacement Versus Fusion: Results of a Prospective, Randomized Clinical Trial. Clin Spine Surg. 2018 Feb;31(1):37-42. doi: 10.1097/BSD.0000000000000476. PMID: 28005616.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
