Tylenol and PRP: Is the Tylenogeddon Warranted?

Credit: Shutterstock
This past few weeks, a new research article suggested that taking Tylenol with a PRP shot may be a bad thing. I’ve been a bit too busy this month to get into this as a blog topic, but with the craziness winding down, it’s time to review this new paper. Let’s dive in.
Why Perform This Extensive Review?
From start to finish, this review of the effects of Tylenol and other medications on PRP took about 6 hours. Why spend this time? Because as the Chief Medical Officer for Regenexx it’s my job to know this stuff cold. It’s also my job to take a deeper dive than most physicians would because our network doctors (and others in the Interventional Orthobiologics community) need an in-depth analysis to make good patient decisions.
PRP
PRP stands for platelet-rich plasma, which is increasingly a “go-to” injection for patients with sports injuries and painful degenerative joints. To learn more, see my video below:
Based on the results of dozens of randomized controlled trials, we know that PRP injections are effective for the treatment of many conditions, including kee arthritis, tendinopathy, and carpal tunnel syndrome.
Medications and PRP
Given that any patient who is a PRP injection candidate could be taking several different medications, it’s reasonable to ask if any of these can impact the outcome of that procedure. I’ll review the research we have; however, realize that the weakness of all of these studies is that they tend to be lab-based and not clinical. Hence impacts noted on platelets in a flask may not necessarily translate into a real impact on everyday results.
Categorizing the Research
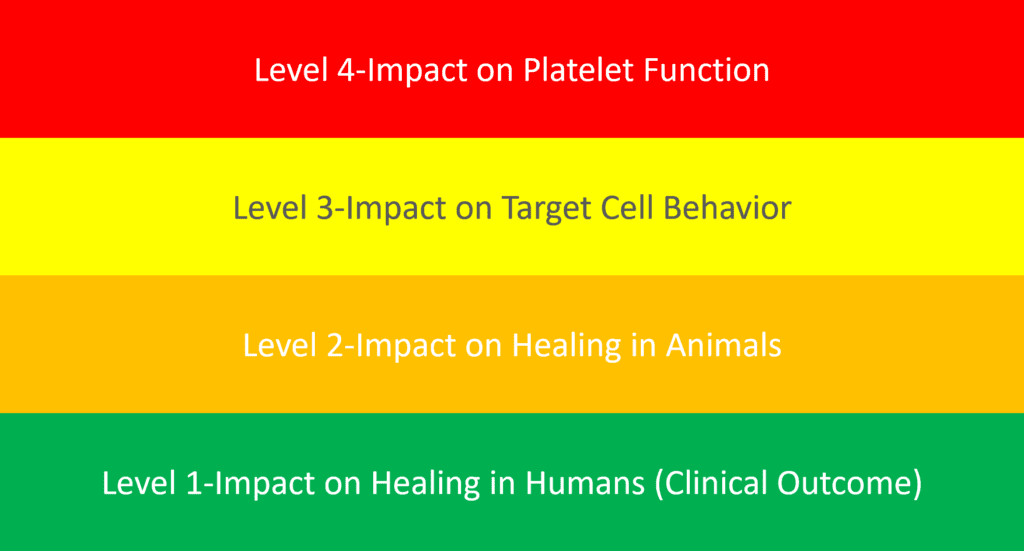
Before we can dig into this topic, we need to categorize this research (see diagram above). Why? Because the quality of the research will determine how much weight we give to it.
Here are some definitions of the research levels I created:
- Level 4—A study where blood is taken from patients where platelet function is measured in the lab. Things like platelet aggregation (how platelets clump together to form a clot) or growth factor release are determined. However, this is not an actual test of the ability of PRP to help stimulate cells to heal.
- Level 3—Research in a culture flask where the ability of PRP to stimulate cells to grow or “heal” is measured. For example, tenocyte cells have the property of closing gaps in culture (called a “scratch test”). A level 3 study would determine whether a medication reduces the ability of PRP to cause tenocytes to close gaps. While this is an actual test of the ability of PRP to stimulate healing, it suffers from the problem of not being performed in a living organism.
- Level 2—An animal study of how PRP can help stimulate healing of a specific injury. For example, researchers give an animal a drug and then measure the ability of PRP to help heal an injured tendon. The limitation here is whether this effect translates to humans.
- Level 1—A human study where researchers study if a drug impacts the clinical outcome of a PRP injection. This could take several forms, from lower-level research like a case series to higher-level randomized controlled trials.
Science is all about replicating results in multiple experiments. Hence, we’re looking for multiple level 1 studies here that all point in the same direction. As you’ll see, we’re not at that point yet. However, let’s dive into what we do know. Note that I grade each study discussed below with that score in [ ].
Corticosteroids
When you hear the phrase “cortisone injection” or “steroid shot,” that usually means a “corticosteroid”. That’s a type of steroid that doesn’t make new muscles (an anabolic steroid) but instead reduces inflammation. Given that doctors may inject a steroid with PRP or a patient can be taking that drug while getting a PRP injection, how does this impact the outcome of that injection? The truth is that nobody is sure.
In one lab-based experiment, local anesthetics and corticosteroids reduced the ability of PRP to help stimulate tendon cells [level 3] (1). In addition, in another lab study, PRP helped protect tendon cells from the adverse effects of corticosteroids and ciprofloxacin (an antibiotic that hurts tendons) [level 3] (2). Finally, methylprednisolone (a commonly used steroid) hurt both cell types in another investigation on both cartilage and tendon cells. However, PRP partially reversed the negative impacts of the steroid [level 3] (5).
As far as clinical studies, we have one that went the other way. Here in knee arthritis patients, using a mega-dose corticosteroid before a PRP injection helped improve outcomes at 3 and 6 months with no difference at 1-year [level 1] (3).
Local Anesthetics
Local anesthetics numb the area to be injected and are often injected with PRP to reduce post-injection pain. As you can see above, one lab study shows that local anesthetics are a problem (1) [level 3]. In another lab-based study, xylocaine and ropivacaine negatively impacted platelet function [level 4] (4). Finally, a 1980s lab study looked at the impact of lidocaine and bupivacaine on platelet function, which reduced platelet aggregation. [level 4] (6).
NSAIDs
NSAIDs are drugs given to patients to reduce pain and inflammation like Motrin, Advil, Alleve, Celebrex, etc… Aspirin (the original NSAID) is well studied to reduce platelet aggregation (clotting time) with multiple lab studies all heading in this direction [level 4] (7). The rank and file non-selective NSAIDs (everything except for Celebrex) also decreased platelet aggregation [level 4] (7). Celebrex, considered a selective COX-2 drug, didn’t impact platelet aggregation. However, we need to be careful here as recent research has shown that these drugs may lead to chronic pain by blocking inflammation, so that would over-rule any impacts on PRP (8). Meaning keeping patients in pain off these drugs is likely a good idea.
The “New” Study
About two weeks ago, the world of Interventional Orthobiologics on Linkedin exploded with the concern that a “new” study demonstrated that Tylenol could severely impact PRP injections. Frankly, this month has been a blur for me with two kids graduating, Mother’s Day, my anniversary, and the loss of a colleague to cancer. Hence, all I could do was try to tread water to keep up. So I initially ignored the frenzied posts and emails on this topic, but after getting yet another email this morning, it was time to dive in.
The new paper everyone is buzzing about is a review on the topic of how various drugs may impact PRP (7). Its conclusion that Tylenol could be a problem is based on a sole paper by Munsterhjelm in 2005 that purported to show that Tylenol (acetaminophen) inhibited platelet aggregation in a dose-dependent manner [level 4] (9).
Reviewing this Munsterhjelm study in-depth, all we find is 13 patients. The good news is that this research is a double-blind cross-over that exposed various patients to a specific IV dose of acetaminophen versus a placebo. The researchers then took blood samples to measure platelet aggregation ability at 10 minutes and 90 minutes after the IV infusion.
One big concern is that this 2005 study used IV acetaminophen. Given that 99.9% of our patients will instead be taking oral Tylenol, the first question is, how do you translate an IV dose to an oral dose? This conversation is where this paper gets really interesting. For example, giving acetaminophen IV results in almost double the blood plasma levels compared to oral (24.9 vs 14.2 μg·h/mL) (10). Hence, when the researchers pushed 15 mg/kg of Tylenol IV, or 1,500 mg in a 225 lb man, that’s equivalent to 2,625 mg of oral Tylenol taken at once! That’s almost a toxic “call poison control” dose which is equal to eight regular strength or five extra-strength pills! These conversions get far worse for the higher doses they used (22.5 mg/kg and 30 mg/kg).
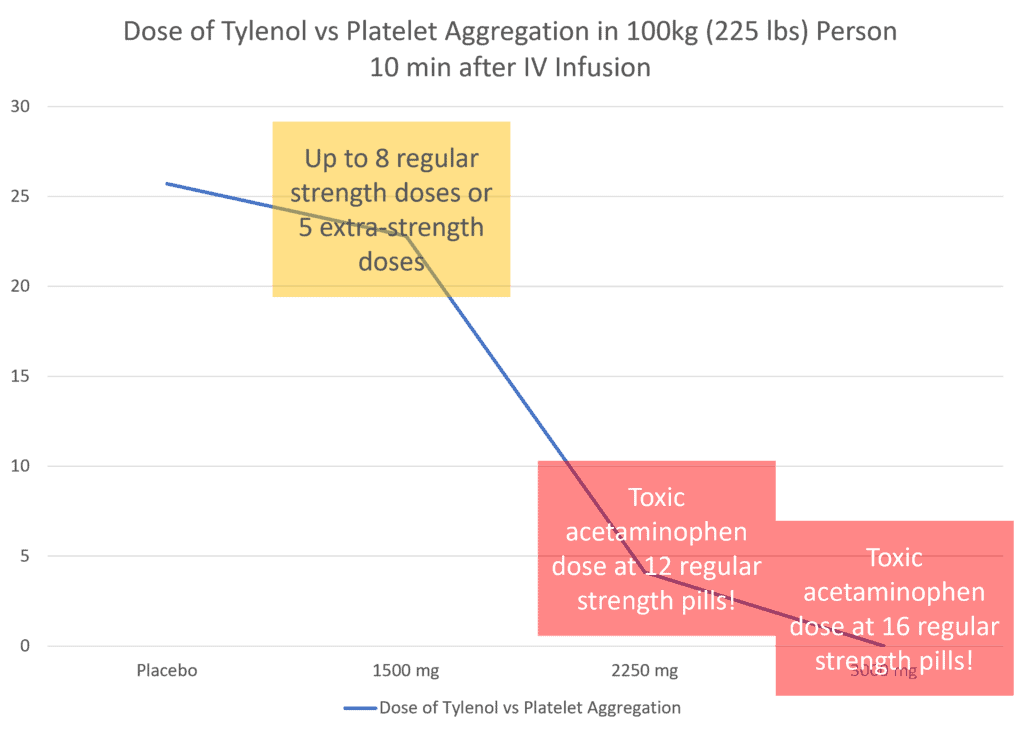
How do these ridiculously high oral Tylenol doses impact platelet aggregation? I created the chart above from the data in the paper. The placebo is on the far left, and the lowest Tylenol dose is in the orange box. The vertical axis here is the amount of platelet aggregation. Note that the aggregation is only slightly off even at this super-high oral dose. It’s also likely that aggregation is closer to normal using regular oral doses of Tylenol. How could Tylenol impact a smaller person than 225 pounds? If we reduce the oral dose to match a 50kg woman, we’re still at four regular strength doses of Tylenol or 2.5 doses of extra-strength. This means that it’s unlikely that a usual and customary dose of oral Tylenol significantly impacts platelets.
The other problem with this study should also be apparent. The doctor injects PRP, and if that comes in contact with free collagen the platelets aggregate and cause a clot to form. Hence, this study only impacts patients walking into a procedure on Tylenol. Taking Tylenol after the fact is not capable of “de-clotting” the blood as that requires specialized drugs. Hence, this study is mute on patients taking Tylenol for pain relief after a PRP injection.
In addition, it gets even less impactful from there. To understand why let’s explore the mechanics of PRP injection. Blood is taken and then re-injected as PRP some 30 minutes to several hours later. In this study, platelet aggregation mostly recovered after 90 minutes. Hence, even if a patient took these near toxic doses of oral Tylenol, the minor hit to platelet aggregation would have mostly recovered by the time the patient was re-injected.
Therefore, this study only really applies to patients who had IV acetaminophen within 10 minutes of when blood is taken, and PRP is prepared and almost immediately re-injected (very uncommon). Or patients who have an IV acetaminophen infusion while being re-injected with PRP. Even then, at usual IV doses, the effect is small.
Finally, this study doesn’t say anything about how Tylenol impacts the effect that PRP has on target cells, its impact on healing in animal models, or any impact on human outcomes.
Conclusions-Is Tylenogeddon Warranted?
NO! The data reported in the 2005 study on the effects of mega-doses of Tylenol on platelet aggregation is NOT concerning. While it may be reasonable to tell patients to stay off Tylenol right before a procedure, there is no contraindication for patients taking the usual doses of Tylenol to control their pain. Also, given the recent data published on NSAIDs causing chronic pain (and NOT Tylenol), I would much rather have my patients on Tylenol.
The upshot? There is no contra-indication to using ordinary Tylenol doses to control pain after a PRP procedure. There are likely minimal impacts on platelet aggregation at the usual doses of Tylenol. More importantly, IMHO, no patient or physician practicing orthobiologics should be freaking out about this most recent publication on Tylenol and PRP.
_______________________________________________
References:
(1) Carofino B, Chowaniec DM, McCarthy MB, Bradley JP, Delaronde S, Beitzel K, Cote MP, Arciero RA, Mazzocca AD. Corticosteroids and local anesthetics decrease positive effects of platelet-rich plasma: an in vitro study on human tendon cells. Arthroscopy. 2012 May;28(5):711-9. doi: 10.1016/j.arthro.2011.09.013. Epub 2012 Jan 21. PMID: 22264830.
(2) Zargar Baboldashti N, Poulsen RC, Franklin SL, Thompson MS, Hulley PA. Platelet-rich plasma protects tenocytes from adverse side effects of dexamethasone and ciprofloxacin. Am J Sports Med. 2011 Sep;39(9):1929-35. doi: 10.1177/0363546511407283. Epub 2011 Jun 1. PMID: 21632978.
(3) Camurcu Y, Sofu H, Ucpunar H, Kockara N, Cobden A, Duman S. Single-dose intra-articular corticosteroid injection prior to platelet-rich plasma injection resulted in better clinical outcomes in patients with knee osteoarthritis: A pilot study. J Back Musculoskelet Rehabil. 2018;31(4):603-610. doi: 10.3233/BMR-171066. PMID: 29710676.
4. Bausset O, Magalon J, Giraudo L, Louis ML, Serratrice N, Frere C, Magalon G, Dignat-George F, Sabatier F. Impact of local anaesthetics and needle calibres used for painless PRP injections on platelet functionality. Muscles Ligaments Tendons J. 2014 May 8;4(1):18-23. PMID: 24932442; PMCID: PMC4049644.
5. Beitzel K, McCarthy MB, Cote MP, Apostolakos J, Russell RP, Bradley J, ElAttrache NS, Romeo AA, Arciero RA, Mazzocca AD. The effect of ketorolac tromethamine, methylprednisolone, and platelet-rich plasma on human chondrocyte and tenocyte viability. Arthroscopy. 2013 Jul;29(7):1164-74. doi: 10.1016/j.arthro.2013.04.006. PMID: 23809450.
6. Borg T, Modig J. Potential anti-thrombotic effects of local anaesthetics due to their inhibition of platelet aggregation. Acta Anaesthesiol Scand. 1985 Oct;29(7):739-42. doi: 10.1111/j.1399-6576.1985.tb02292.x. PMID: 4072600.
(7) Kao, David S et al. “A Systematic Review on the Effect of Common Medications on Platelet Count and Function: Which Medications Should Be Stopped Before Getting a Platelet-Rich Plasma Injection?.” Orthopaedic journal of sports medicine vol. 10,4 23259671221088820. 12 Apr. 2022, doi:10.1177/23259671221088820
(8) Parisien M, Lima LV, Dagostino C, El-Hachem N, Drury GL, Grant AV, Huising J, Verma V, Meloto CB, Silva JR, Dutra GGS, Markova T, Dang H, Tessier PA, Slade GD, Nackley AG, Ghasemlou N, Mogil JS, Allegri M, Diatchenko L. Acute inflammatory response via neutrophil activation protects against the development of chronic pain. Sci Transl Med. 2022 May 11;14(644):eabj9954. doi: 10.1126/scitranslmed.abj9954. Epub 2022 May 11. PMID: 35544595.
(9) Munsterhjelm E, Munsterhjelm NM, Niemi TT, Ylikorkala O, Neuvonen PJ, Rosenberg PH. Dose-dependent inhibition of platelet function by acetaminophen in healthy volunteers. Anesthesiology. 2005 Oct;103(4):712-7. doi: 10.1097/00000542-200510000-00009. PMID: 16192763.
(10) Singla NK, Parulan C, Samson R, Hutchinson J, Bushnell R, Beja EG, Ang R, Royal MA. Plasma and cerebrospinal fluid pharmacokinetic parameters after single-dose administration of intravenous, oral, or rectal acetaminophen. Pain Pract. 2012 Sep;12(7):523-32. doi: 10.1111/j.1533-2500.2012.00556.x. Epub 2012 Apr 24. PMID: 22524979.
.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
