Understanding How Physicians Keep Their Families Safe -The Ladder

My wife this past weekend fractured her fibula so my week was taken up by being a patient’s husband. One of the things that I think many patients need to understand is how we physicians look at medical care for our own family members. One of the rules we always follow is “the ladder”. Which ladder and how can that protect you just like it protects our spouses and kids? Let’s dig in.
Being a Patient
One of the best experiences that a physician can have is to be a patient or connected to someone who is a patient. Why? It gives us insight into what our patients endure day in and day out.
This past weekend my wife got caught up in one of the dogs and fell onto her ankle, which fractured the distual fibula (small bone on the outside of the leg). On the one hand, having a physician husband meant that she was in a privledged position with help navigating the medical care system. However, her real advantage was that by living with me for decades she had already been schooled in “the ladder” which meant that she was already innoculated against the worst the medical care system could dish out.
What Is “The Ladder”?
How do physicians look at medical care for their own families? They use “the ladder”. What’s that?
If you want to keep patients as safe as possible, you only expose them to the least risk needed to get the job done. That system creates a ladder that looks like this:
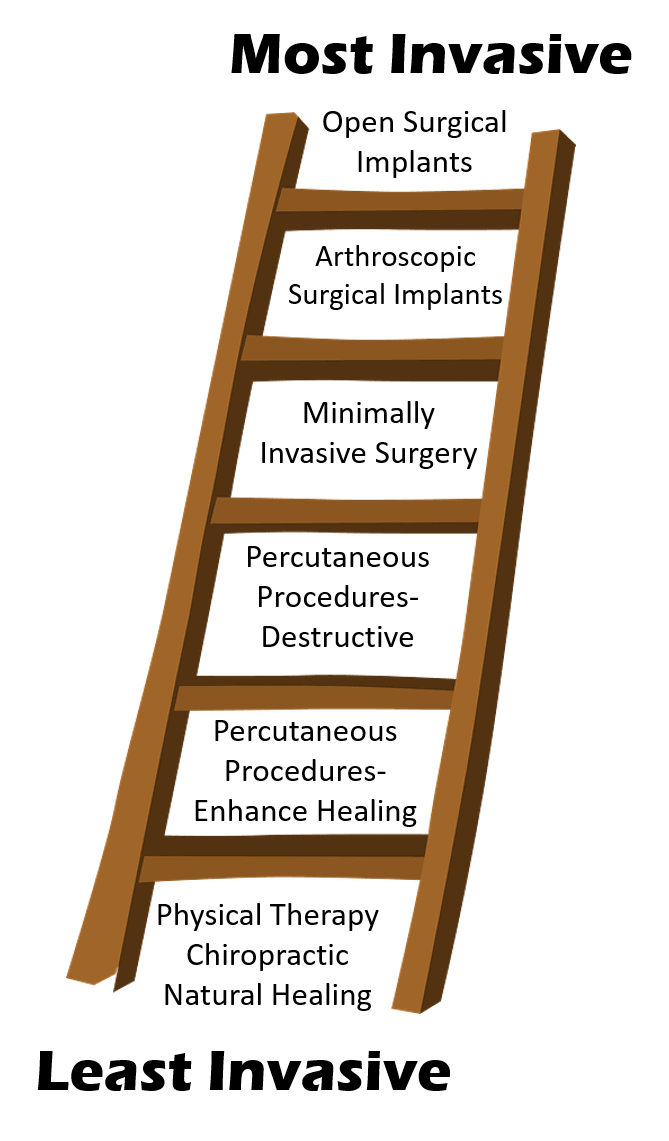
You’ll notice at the bottom is conservative care. Things like physical therapy, chiropractic, or other natural healing alternatives should always come first. My wife chose to get her leg casted, which is what used to happen for all patients when I was a kid. However, she had at least one surgeon tell her that she needed surgery to place a plate. Another more honest surgeon told her she could get it casted or get a plate. She went with the second guy.
Next up are percutaneous procedures that can promote healing. That’s what we do with interventional orthobiologics. Percutaneous means “through the skin” meaning that no surgery is involved. So that’s placing substances using needles that promote healing by using precise imaging guidance. For example, a fluoroscopy guided PRP or stem cell procedure to heal a torn ACL
Next up are percutaneous destructive procedures. For example, a patient with spinal pain who gets a radiofrequency ablation which destroys the painful nerve. Or a patient with neck pain who gets botox injected, which destroys or injures the neuromuscular junction. These procedures carry more risk since they destroy rather than heal tissue.
One step up the ladder is minimally invasive surgery. So again for a spine patient, this would be working through a smaller hole and scope system to remove small amounts of bone or disc that could be trapping a nerve. Or a knee problem that can be surgically repaired through suturing with an arthroscope. This has more risk than injections, but less risk than bigger surgeries.
Next up are procedures that implant something. These surgeries can still be done through a scope, but some implant is placed. Since the implant can move out of place and wreck havoc on the body or the body can react to the implant, this means that these procedures are more invasive. This would also include quasi-surgical procedures that place an implant into the body.
Finally, at the top of the list are open surgical implants. These are procedures like fusion where screws or rods or plates are placed to make sure parts of the spine or a joint can never move again. The same risks are there as above, but now you add the risk of open surgery. In addition, you add the risks of things like adjacent segment disease, where the levels or joints above and below get chronically injured due to the fusion.
Moving Up or Down the Ladder
Obviously there are procedures that don’t fit perfectly in the ladder. For example, you can move up the ladder with a percutaneous fusion device. That has risk that’s more a cross between a surgical fusion and a percutaneous procedure. A good example there is SI fusion using a screw or dowel system that’s implanted without open surgery. Or a device implant like Vertiflex which is used to help patients who have spinal stenosis. That’s a percutaneous procedure (more like a scope level of destruction), but something is left in the body, so the risk is much higher than a percutaneous destructive procedure like radiofrequency ablation.
Here’s a Facebook live I did on this topic:
Keeping Yourself Safe: How Do Physicians Look at Surgery for Their Own Families?
Posted by Regenexx on Friday, January 29, 2021
Thinking Like a Doctor Protecting His Family
So how can you use the ladder like I would to protect my wife or kids? Anything lower on the ladder that applies to that injury or problem that may work needs to be tried first before moving up the ladder. That way you don’t get exposed to more risk than you need.
Accepting Medical Risks
To really understand and use the ladder to reduce and manage your risk, you avoid signing up for the first thing offered. What I mean is that doing your homework can help you understand all of the possible options to fill in your personal ladder. To get there you need to spend several hours online digging deep to find out all of the options your doctor knows about and would consider if this were his wife or kid.
The upshot? So if you want to keep yourself safe, you need to understand and use the ladder. While there are times that the most invasive thing needs to be done, they are generally few and far between. Usually, less invasive options are available and will often work. It may, however, take some homework!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
