What Does Treating Hip AVN without Surgery Have to Do with the History of Orthobiologics?
Many of the advanced interventional orthobiologics procedures currently used in peripheral joints and spine were developed by our Colorado HQ. That led to the creation of the Interventional Orthobiologics Foundation (IOF) which has continued to teach and evolve these breakthrough procedures. However, one procedure that we didn’t develop is the precise x-ray-guided injection of bone marrow concentrate to treat avascular necrosis of the hip. This morning we’ll go over a recent patient we helped using this technique and peruse a bit of orthobiologics history at the same time.
Creating Interventional Orthobiologics
Back in 2005, our clinic began investigating how one might use culture-expanded mesenchymal stem cells and bone marrow concentrate to help patients avoid the need for invasive orthopedic surgery. Nobody else on earth was using an image-guided needle-based procedure to treat common orthopedic problems like ligament tears and low back DDD, so everything we developed using fluoroscopy and ultrasound-guided injections was new. For example, how should BMC be injected into a damaged ACL to help it heal? There was no textbook or publication that described this procedure. As far as we knew, no other human had ever tried to do this. We took 2-3 years to develop it ourselves using trial and error, studying anatomy, trying different image-guided techniques, and eventually dialing in a procedure that worked every time. So if you’re a physician who has been taught how to inject this ligament using fluoroscopy or ultrasound, you have us to thank, as we did that groundbreaking work that has now led to a number of peer-reviewed publications (1-3).
However, way back when, there was someone who was more experienced than our clinic in treating bone disease in Paris, France. Phillipe Hernigou is an orthopedic surgeon who used bone marrow concentrate to treat AVN and delayed healing fractures while I was still in medical school and residency. (4,5). Hence, we didn’t develop the procedure to treat AVN without surgery but followed Phillipe’s expert lead. In fact, the basic idea that we could use BMC or culture-expanded MSCs to treat orthopedic conditions came from Phillipe’s published works on treating bone disease.
What is AVN?
AVN means Avascular Necrosis which is a bone disease most commonly impacting the hips. Basically, the progenitor cells that repair bone get sick and can’t keep up with the normal wear and tear we all encounter. Hence, the bone begins to die off and if left alone will predictably collapse, often requiring a hip replacement. This disease is also called osteonecrosis.
The treatment, if caught early, is a drilling technique where the surgeon begins on the side of the femur and drills a large tunnel into the femoral head. The idea was that this was ‘decompressing” the AVN lesion (dead bone), but that’s a 1960s conceptualization of what’s wrong. Instead, the procedure likely drags healthy bone marrow and working bone repair cells into the bad area. Hernigou was the first physician to figure out that if you replaced the drill with a long bone needle (trocar) and injected healthy bone marrow from another spot, you could skip the big surgery.
Our Latest Patient
Since 2005, we’ve helped many hip AVN patients avoid the need for invasive surgery using the Hernigou bone marrow concentrate injection technique. This is our latest.
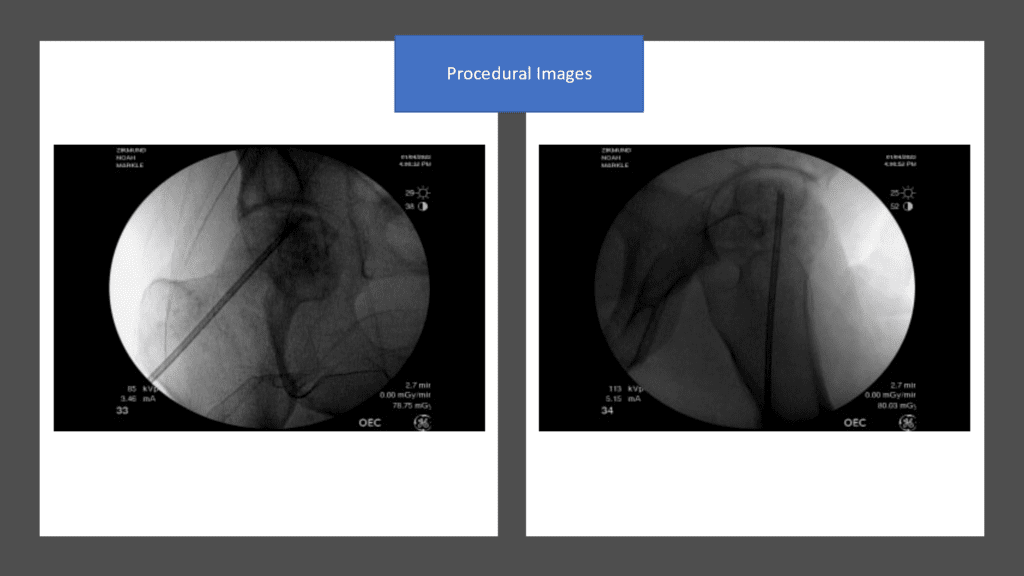
Dr. Markle first evaluated this 45-year-old college professor 6 months ago after he had seen an orthopedic surgeon who was planning to perform surgery. The patient was told that he had ARCO grade 2 hip AVN and possibly early sage 3. Given that the patient wanted to avoid surgery, Dr. Markle used the Hernigou technique to place long trocars with fluoroscopy guidance into the AVN lesions and injected the patient’s own high-dose bone marrow concentrate:
Here are the before and after images:
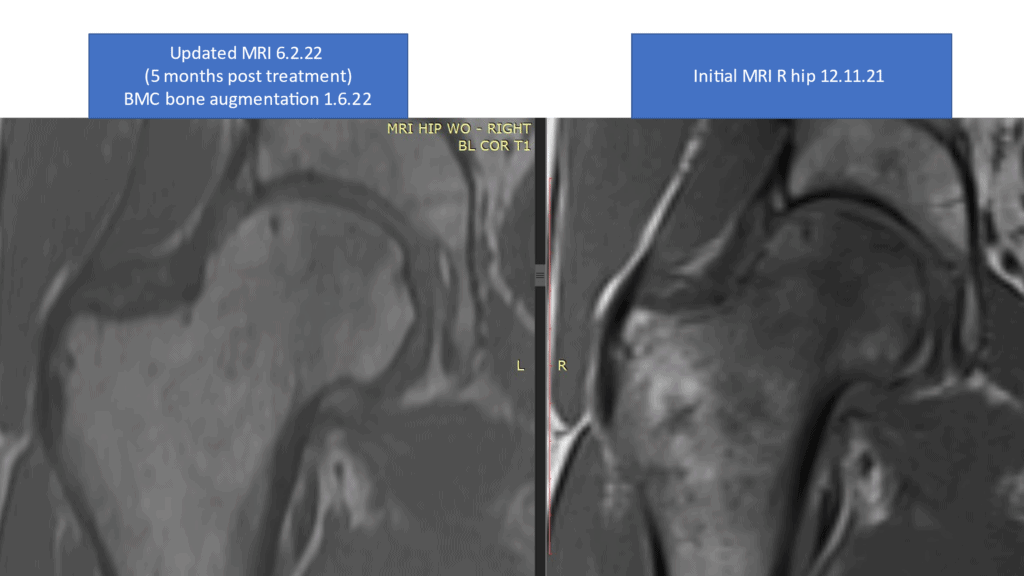
The image on the left above (5 months after treatment) shows a normal hip from the front (coronal), which on this type of MRI sequence should be light in color (normal bone is white). The before procedure image on the right showing dark bone means that the tissue is dying (AVN).
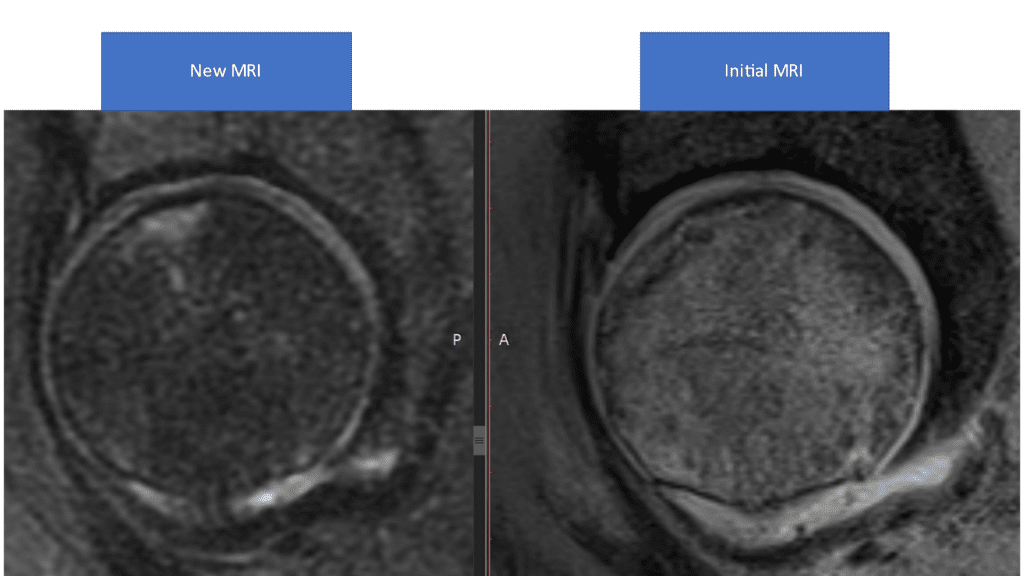
The image on the left above shows a mostly normal hip from the side (sagittal). The bone in this type of MRI sequence should be dark. The small amount of bright signal means that a little bit of the bone has yet to fully heal some 5 months after the procedure. The before procedure image on the right showing bright bone means that the tissue is dying (AVN).
Given that symptomatically the patient is doing well, he has likely successfully avoided a big orthopedic surgery and/or hip replacement.
The upshot? We’ve developed many of the advanced interventional orthobiologics procedures in use today. However, way back in 2005 when we began figuring this all out, we also got to stand on the shoulders of giants like Phillipe Hernigou who had already figured out how to treat hip AVN with an injection of BMC rather than more invasive surgery. Hence, we’re not above using Phillipe’s technique to help our patients avoid the need for a hip replacement!
_______________________________________
References:
(1) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437–447. https://www.ncbi.nlm.nih.gov/pubmed/26261424
(2) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. https://www.ncbi.nlm.nih.gov/pubmed/30176875
(3) Centeno C, Lucas M, Stemoer I, Dodson E. IMAGE-GUIDED INJECTION OF ANTERIOR CRUCIATE LIGAMENT TEARS WITH AUTOLOGOUS BONE MARROW CONCENTRATE AND PLATELETS: MIDTERM ANALYSIS FROM A RANDOMIZED CONTROLLED TRIAL. Bio Ortho J Vol 3(1):e29–e39; October 5, 2021.
(4) Hernigou P, Poignard A, Zilber S, Rouard H. Cell therapy of hip osteonecrosis with autologous bone marrow grafting. Indian J Orthop. 2009 Jan;43(1):40-5. doi: 10.4103/0019-5413.45322. PMID: 19753178; PMCID: PMC2739495.
(5) Hernigou P, Mathieu G, Poignard A, Manicom O, Beaujean F, Rouard H. Percutaneous autologous bone-marrow grafting for nonunions. Surgical technique. J Bone Joint Surg Am. 2006 Sep;88 Suppl 1 Pt 2:322-7. doi: 10.2106/JBJS.F.00203. PMID: 16951103.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
