What Is Degenerative Spondylolisthesis? I and Many Patients Are in a Race Against Time
Eventually, all doctors get to be patients. I'm no different. Recently an X-ray of my back showed that I'm in a race against time and gravity. Let me explain.
Being a Patient
If you read this blog, you may know that I have a back condition. Mine began when I flipped a Jeep while in residency training. I broke three transverse processes in my spine (the side projections on the vertebrae). I have intermittent back pain and left-sided irritated spinal nerves (S1 radiculopathy).
My back has been successfully managed by my colleagues at our Colorado HQ for years. I'm very active, left heavy weights, and have few functional limitations (although I don't run anymore). Once or twice a year, I get on the table, just like my patients, and put my back in the hands of another physician. Recently, that physician noted that the L5 vertebra had just begun to slip forward on the tailbone (sacrum), so what's happening, and why is that a race against time and gravity?
What Is Degenerative Spondylolisthesis?
The spine bones stack one on top of the other as shown below. When one bone slips forward on the other, this is called spondylolisthesis. This can happen when the bones are created at birth without the right connection, or with wear and tear. The latter is called degenerative spondylolisthesis.
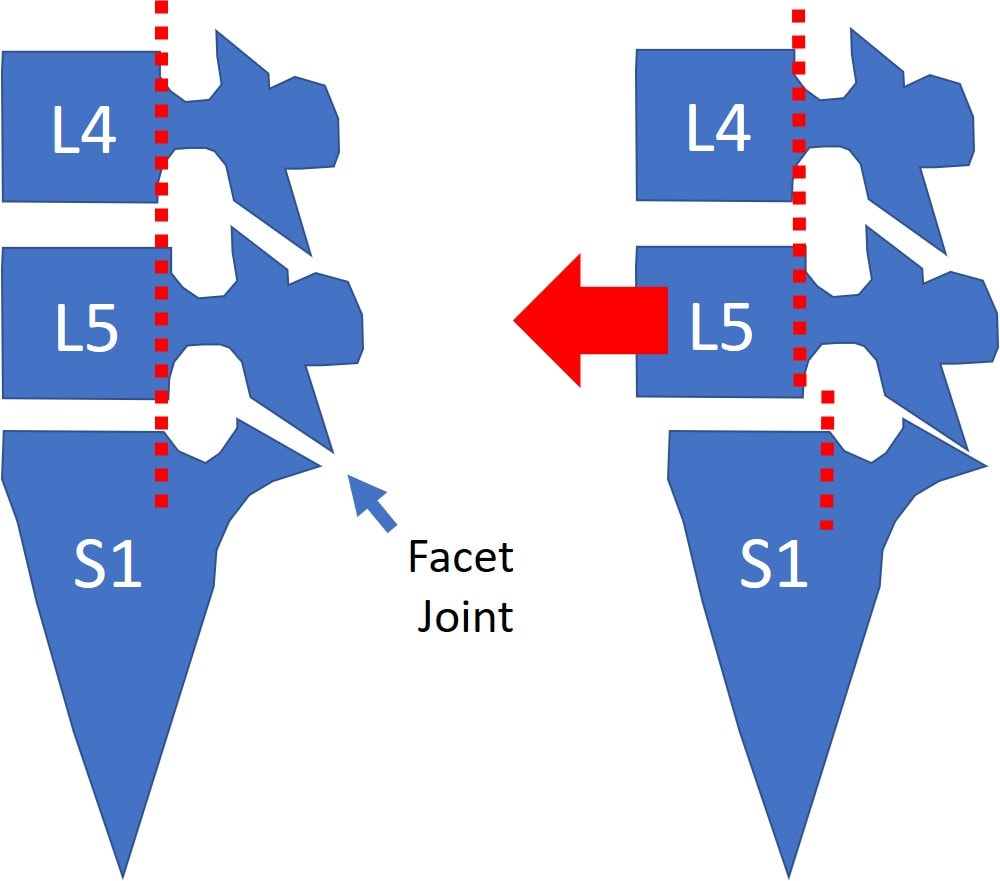
Note that the facet joint in the back of the spine is what usually prevents one vertebra from slipping forward on the next. So a degenerative spondylolisthesis happens because the facet joint gets arthritic and misshapen, which no longer holds the top vertebra back on the bottom bone. So what's the big deal?
The Consequences of Degenerative Spondylolisthesis
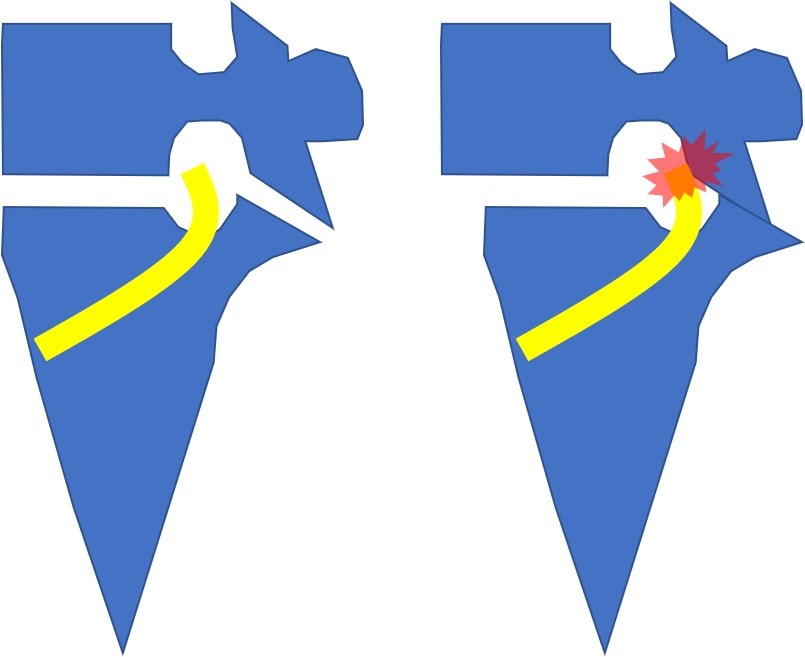
The nerves that power your legs and take sensation from there to your brain must pass through the hole that's formed between the two vertebrae. That hole is called a foramen, and you can see that on the left below (nerve is yellow). On the right, note that as one vertebra slips forward on the other, the hole gets smaller and pinches the nerve. The facet joint can also get arthritic and larger, which can cause more pressure. Finally, the disc that lives between the two vertebrae can also get damaged, leading to a disc bulge which can also further irritate the nerve.
How Can We Fix Degenerative Spondylolisthesis?
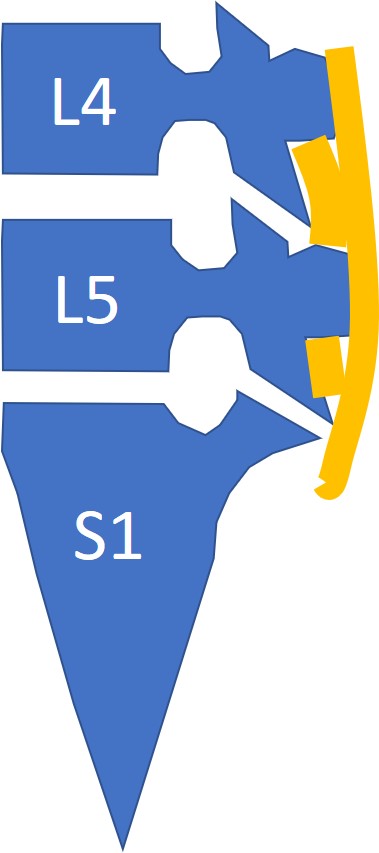
Note that the ligaments (orange) in the back of the spine are sort of like pieces of duct tape. These are called the supraspinous and interspinous ligaments, and they and other ligaments (iliolumbar) can provide resistance to the forward movement. So in addition to bad facet joints, loose ligaments can also cause a degenerative spondylolisthesis. Hence, we often target these ligaments in a precise image-guided procedure called a percutaneous ligamentoplasty. These can be injected with either platelets or stem cells to build tougher and thicker ligaments.
Why Is This a Race Against Time and Gravity?
Catching a degenerative spondylolisthesis early is critical. Why? Because the spine is tilted forward, and since we all tend to live our lives in front of our spine, the vertebrae usually fall further forward. The more the vertebra gets out of whack, the harder this problem is to fix with injections.
So What Have I Done and What Do I Recommend For My Patients?
This problem was identified a few weeks ago, and I underwent my first percutaneous ligamentoplasty with platelets at that time. I'll also pull the trigger on a second one when I return to Colorado and likely once a month for the next several months. Why am I hitting it so hard? Because the farther the vertebra moves forward, the more distorted the facet joint will become and the harder this will be to fix without surgery. Hence, I have to get on top of this, and if you're a patient with this issue, I also recommend that you get this aggressively treated.
The upshot? I actually love being a patient because it teaches me how to be a better doctor. Why? Because what I need to do for myself is what I need to recommend for my patients. In this case, it's to get these ligaments as tight as possible as quickly as possible so I and my patients can win that contest with time and gravity!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
