What Is PRGF?
Credit: Shutterstock
A new treatment called PRGF seems to have become popular this past year with physicians using orthobiologics. What is it? What’s it used for? What’s the evidence behind it? Why should you care? Let’s dig in?
What’s the Buzz About?
I was recently listening to a number of physicians who use orthobiologics discuss PRGF. There seemed to be an unusual buzz around it, so in my job as Chief Medical Officer for Regenexx, I have to investigate and learn what’s up. Since I do that by blogging, you’re coming along for the ride this morning as I perform a deep dive.
As I began this review yesterday, I really didn’t know much about the product. Hence, you’ll learn right along with me as I go deep into this topic.
What Is PRGF?
PRGF stands for Plasma Rich in Growth Factors. There is a specific company called Endoret out of Spain that has a trademark on PRGF and that holds patents on the kits that doctors use to create the product. That company is also associated with both BTI (Biotechnology Institute) and the Eduardo Anitua Institute. The product has historically been used in dentistry and dental implants.
PRGF is made very similarly to PRP in that blood is placed in a blood collection tube containing anti-coagulant (ACD). That blood is then spun in a centrifuge to push the red and white blood cells toward the bottom half of the tube and keeping the plasma and platelets just above that layer. The platelet-rich layer just above the red cells is then collected. When used for injection this can be injected as a leukocyte-poor PRP (LP-PRP) and when used in surgery, it can be activated with calcium chloride and turned into a clot creating platelet-rich fibrin (PRF).
Not knowing much about how PRGF was made, I was a bit surprised that nothing about it seemed at all different than a commonly used method for making for either LP-PRP or PRF. Hence, my review so far doesn’t explain the hype. Hence, time to dig deeper.
What’s In PRGF?
A paper by Nishiyama analyzed PRGF (1). What’s in it? It’s basically a 3X LP-PRP. What does that mean? Platelet-rich plasma concentrates blood platelets. Your blood begins with 1X platelets, so a 3X PRP has three times as many platelets as was in the whole blood. That’s a pretty weak PRP. Meaning most bedside kit systems that many doctors use can concentrate platelets to 5-7X over baseline. We routinely concentrate them to 7-20X in the lab. Why does this matter? Let’s look at our recent paper on how concentration impacted how well tendon cells were able to grow and heal a defect (2):
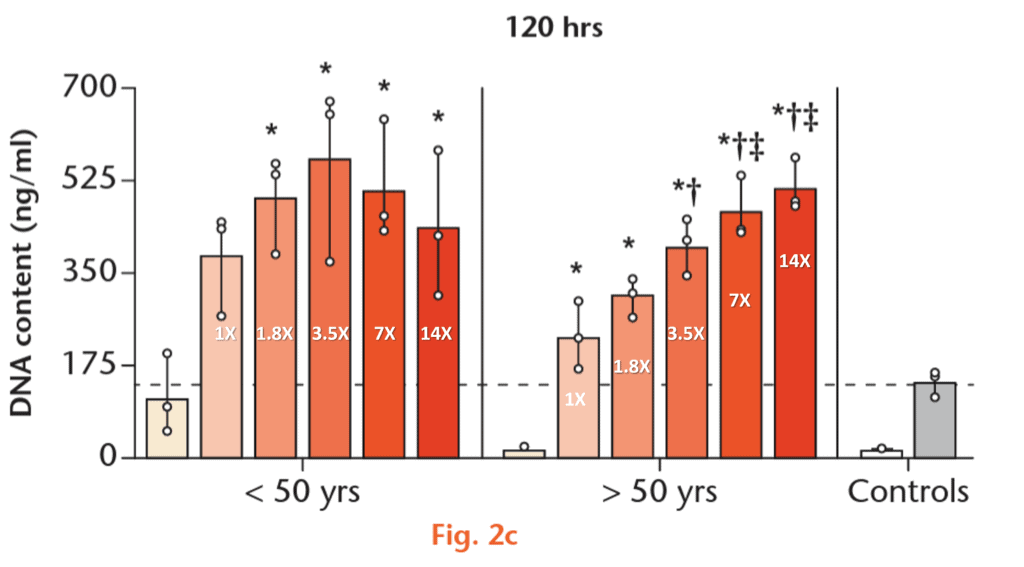
Note that when you’re in your 20s and 30s (under 50 yrs here to the left) increasing the concentration of PRP beyond 3.5X doesn’t help much. In this graph, the higher the bar the better PRP helped the tendon cells heal. However, when you get older (the graph to the right), the higher the concentration, the more healing you get, here shown up to 14X. In fact, we have shown the same thing all the up to 20X. Given that most people getting PRP in the US are older as that’s when various parts and pieces really start going bad, concentration is key.
So why all the hype about PGRF? Maybe it’s something else? Let’s dig even deeper.
Does PGRF Stimulate Cells Better than PRP?
The Nishiyama paper above suggests that PRGF stimulates periodontal cells (very similar to the tenocytes above) better than PRP. However, there are all sorts of problems with that claim. Let’s dig in.
First, the authors made their own periodontal cells from the teeth of volunteers, but don’t tell us their age. Why is that critical to know? Look at the graph above. If the patients were younger (which is likely since this study was performed at a dental school and students are often the volunteers for lab studies), then the 3X PRGF would be expected to perform well and the almost 9X PRP they prepared would be expected to underperform (graph on the left). However, increase the age of the volunteers and you would get the opposite result (graph on the right).
Second, the PRP made by the authors was red and white blood cell rich, which we have seen decreases proliferation of cells in culture. We’ve often theorized that the extra red cells and their breakdown products could be toxic in the closed system of cell culture. Hence, we have no idea what would have happened if the authors made 9X LP-PRP which would have been an apples-to-apples comparison since PRGF is a LP-PRP.
What Else Is Published On the Basic Science Behind PRGF?
The company that makes the PRGF has published a paper on the proteins in the resulting platelet-rich fibrin clot that’s used in surgery (4). Other papers have also been published. This one extols the virtues of leaving out the white blood cells (leukocytes) from PRGF (58). However, given that more than half of all of the PRP used these days is leukocyte poor (LP-PRP), that’s not so unique in the 2020s.
How Much Clinical Data Is there Supporting the Use of PRGF?
One of the mysteries of why there is such hype around PRGF are the dozens of randomized controlled trials showing that PRP works (5-54). Meaning, as I recently listened to one physician extoll his opinion of the magical properties of PRGF, my mind went to one thought-why switch horses from tried, true, and extensively tested PRP to PRGF?
So are there dozens of randomized control trials on PRGF compared to the four dozen-plus on PRP? I found two RCTs where the company compared PRGF to hyaluronic acid injections to treat knee osteoarthritis (56,57). At 6-months, PRGF was better, which is what would have been expected for a 3X LP-PRP, as 18 studies have compared PRP to HA for knee OA and have shown the superiority of PRP over HA. I also found a small case series and opinion piece extolling the virtues of PRGF in a surgical bone healing application (55).
After that literature search, I continued to be stupefied about the hype around PRGF.
PRGF Gets Called Out by Scientists
What I had never seen before was a 2014 editorial I came across when researching PRGF for this blog. The founder of the company that makes the PRGF kits (Anitua who founded the company Endoret), was called out by scientists who were tired of his claims about the fantastic properties of PRGF (3). I had never seen anything quite like this in the medical literature:
“These authors rarely disclosed all their conflicts of interest since the beginning of the PRGF® story5. In most articles from this group, no disclosure of interest was clearly spelled, even though, in this case, the conflicts of interest cannot be bigger. After a few conflicts that highlighted this reality5, these authors were also using the affiliation “Eduardo Anitua Foundation for Biomedical Research”, while it is obvious that this entity is heavily conflicted by commercial interests like BTI. We will voluntarily not cite any references from this group for the reason explained further in this letter, but they are easy to find on Pubmed and in other electronic databases.”
The accusation was that in papers published by the company, there was often inadequate disclosure that the research was performed by the company making the PRGF kit. This editorial was apparently prompted by the authors writing a paper on classifying PRP preparations that Dr. Anitua felt didn’t reference enough of the company’s published work.
My PRGF Conclusions?
PRGF is nothing more than a low-concentration 3X LP-PRP that can be made into a platelet-rich fibrin clot just like any PRP can be by adding calcium chloride. I can find no evidence of magical healing properties. In fact, while this would be a good product to use in a young patient with a tendon or other issue, in older patients, the platelet concentration, based on the existing in-vitro data is far too low.
The upshot? Whenever I hear a product is magical, I dig deep to find out what’s up. Why? Because while orthobiologics in many ways are a game-changer, none of them are magic. When the right orthobiologic product is used in the right way, by a doctor with the right training, and in the right patient, we can help patients avoid invasive orthopedic surgery. However, claims of fantastic properties do more to set the field back than advance it.
_________________________________________________________
References:
(1) Nishiyama K, Okudera T, Watanabe T, Isobe K, Suzuki M, Masuki H, Okudera H, Uematsu K, Nakata K, Kawase T. Basic characteristics of plasma rich in growth factors (PRGF): blood cell components and biological effects. Clin Exp Dent Res. 2016 Mar 18;2(2):96-103. doi: 10.1002/cre2.26. PMID: 29744155; PMCID: PMC5839250.
(2) Berger DR, Centeno CJ, Steinmetz NJ. Platelet lysates from aged donors promote human tenocyte proliferation and migration in a concentration-dependent manner. Bone Joint Res. 2019 Feb 2;8(1):32-40. doi: 10.1302/2046-3758.81.BJR-2018-0164.R1. PMID: 30800297; PMCID: PMC6359887.
(3) Dohan Ehrenfest DM, Zhang CQ, Pinto NR, Bielecki T. Merchants shall be expelled from the Temple: the PRGF(®) (Plasma-Preparation Rich in Growth Factors)-Endoret(®) case. Muscles Ligaments Tendons J. 2015;4(4):473-477. Published
(4) Anitua E, Prado R, Azkargorta M, Rodriguez-Suárez E, Iloro I, Casado-Vela J, Elortza F, Orive G. High-throughput proteomic characterization of plasma rich in growth factors (PRGF-Endoret)-derived fibrin clot interactome. J Tissue Eng Regen Med. 2015 Nov;9(11):E1-12. doi: 10.1002/term.1721. Epub 2013 Mar 18. PMID: 23505226.
(5) Senna MK, Shaat RM, Ali AAA. Platelet-rich plasma in treatment of patients with idiopathic carpal tunnel syndrome. Clin Rheumatol. 2019 Dec;38(12):3643-3654. doi: 10.1007/s10067-019-04719-7. Epub 2019 Aug 16. PMID: 31420812.
(6) Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med. 2013 Nov;41(11):2609-16. doi: 10.1177/0363546513496542. Epub 2013 Jul 26. PMID: 23893418.
(7) Malahias MA, Nikolaou VS, Johnson EO, Kaseta MK, Kazas ST, Babis GC. Platelet-rich plasma ultrasound-guided injection in the treatment of carpal tunnel syndrome: A placebo-controlled clinical study. J Tissue Eng Regen Med. 2018 Mar;12(3):e1480-e1488. doi: 10.1002/term.2566. Epub 2017 Dec 17. PMID: 28873284.
(8) Malahias MA, Nikolaou VS, Johnson EO, Kaseta MK, Kazas ST, Babis GC. Platelet-rich plasma ultrasound-guided injection in the treatment of carpal tunnel syndrome: A placebo-controlled clinical study. J Tissue Eng Regen Med. 2018 Mar;12(3):e1480-e1488. doi: 10.1002/term.2566. Epub 2017 Dec 17. PMID: 28873284.
(9) Uslu Güvendi E, Aşkin A, Güvendi G, Koçyiğit H. Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis. Arch Rheumatol. 2017;33(3):273–281. Published 2017 Nov 2. doi: 10.5606/ArchRheumatol.2018.6608
(10) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(11) Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017;5(2):2325967116689386. Published 2017 Feb 13. doi: 10.1177/2325967116689386
(12) Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee Osteoarthritis Injection Choices: Platelet- Rich Plasma (PRP) Versus Hyaluronic Acid (A one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. Published 2015 Jan 7. doi: 10.4137/CMAMD.S17894
(13) Montañez-Heredia E, Irízar S, Huertas PJ, et al. Intra-Articular Injections of Platelet-Rich Plasma versus Hyaluronic Acid in the Treatment of Osteoarthritic Knee Pain: A Randomized Clinical Trial in the Context of the Spanish National Health Care System. Int J Mol Sci. 2016;17(7):1064. Published 2016 Jul 2. doi: 10.3390/ijms17071064
(14) Görmeli G, Görmeli CA, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017 Mar;25(3):958-965. doi: 10.1007/s00167-015-3705-6.
(15) Lana JF, Weglein A, Sampson SE, et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016;12(2):69–78. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227106/
(16) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(17) Lin KY, Yang CC, Hsu CJ, Yeh ML, Renn JH. Intra-articular Injection of Platelet-Rich Plasma Is Superior to Hyaluronic Acid or Saline Solution in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized, Double-Blind, Triple-Parallel, Placebo-Controlled Clinical Trial. Arthroscopy. 2019 Jan;35(1):106-117. doi: 10.1016/j.arthro.2018.06.035.
(18) Huang Y, Liu X, Xu X, Liu J. Intra-articular injections of platelet-rich plasma, hyaluronic acid or corticosteroids for knee osteoarthritis : A prospective randomized controlled study. Orthopade. 2019 Mar;48(3):239-247. doi: 10.1007/s00132-018-03659-5.
(19) Di Martino A, Di Matteo B, Papio T, Tentoni F, Selleri F, Cenacchi A, Kon E, Filardo G. Platelet-Rich Plasma Versus Hyaluronic Acid Injections for the Treatment of Knee Osteoarthritis: Results at 5 Years of a Double-Blind, Randomized Controlled Trial. Am J Sports Med. 2019 Feb;47(2):347-354. doi: 10.1177/0363546518814532.
(20) Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018;16(3):2119–2125. doi: 10.3892/etm.2018.6412
(21) Buendía-López D, Medina-Quirós M, Fernández-Villacañas Marín MÁ. Clinical and radiographic comparison of a single LP-PRP injection, a single hyaluronic acid injection and daily NSAID administration with a 52-week follow-up: a randomized controlled trial. J Orthop Traumatol. 2018;19(1):3. Published 2018 Aug 20. doi: 10.1186/s10195-018-0501-3
(22) Su K, Bai Y, Wang J, Zhang H, Liu H, Ma S. Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis. Clin Rheumatol. 2018 May;37(5):1341-1350. doi: 10.1007/s10067-018-3985-6.
(23) Louis ML, Magalon J, Jouve E, Bornet CE, Mattei JC, Chagnaud C, Rochwerger A, Veran J3, Sabatier F. Growth Factors Levels Determine Efficacy of Platelets Rich Plasma Injection in Knee Osteoarthritis: A Randomized Double Blind Noninferiority Trial Compared With Viscosupplementation. Arthroscopy. 2018 May;34(5):1530-1540.e2. doi: 10.1016/j.arthro.2017.11.035.
(24) Lisi C, Perotti C, Scudeller L, Sammarchi L, Dametti F, Musella V, Di Natali G. Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A randomized controlled trial. Clin Rehabil. 2018 Mar;32(3):330-339. doi: 10.1177/0269215517724193
(25) Cole BJ, Karas V, Hussey K, Pilz K, Fortier LA. Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis. Am J Sports Med. 2017 Feb;45(2):339-346. doi: 10.1177/0363546516665809.
(26) Kaminski R, Maksymowicz-Wleklik M, Kulinski K, Kozar-Kaminska K, Dabrowska-Thing A, Pomianowski S. Short-Term Outcomes of Percutaneous Trephination with a Platelet Rich Plasma Intrameniscal Injection for the Repair of Degenerative Meniscal Lesions. A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study. Int J Mol Sci. 2019 Feb 16;20(4):856. doi: 10.3390/ijms20040856. PMID: 30781461; PMCID: PMC6412887.
(27) Malahias MA, Roumeliotis L, Nikolaou VS, Chronopoulos E, Sourlas I, Babis GC. Platelet-Rich Plasma versus Corticosteroid Intra-Articular Injections for the Treatment of Trapeziometacarpal Arthritis: A Prospective Randomized Controlled Clinical Trial. Cartilage. 2021 Jan;12(1):51-61. doi: 10.1177/1947603518805230. Epub 2018 Oct 20. PMID: 30343590; PMCID: PMC7755966.
(28) Dallari D, Stagni C, Rani N, Sabbioni G, Pelotti P, Torricelli P, Tschon M, Giavaresi G. Ultrasound-Guided Injection of Platelet-Rich Plasma and Hyaluronic Acid, Separately and in Combination, for Hip Osteoarthritis: A Randomized Controlled Study. Am J Sports Med. 2016 Mar;44(3):664-71. doi: 10.1177/0363546515620383. Epub 2016 Jan 21. PMID: 26797697.
(29) Battaglia M, Guaraldi F, Vannini F, Rossi G, Timoncini A, Buda R, Giannini S. Efficacy of ultrasound-guided intra-articular injections of platelet-rich plasma versus hyaluronic acid for hip osteoarthritis. Orthopedics. 2013 Dec;36(12):e1501-8. doi: 10.3928/01477447-20131120-13. PMID: 24579221.
(30) Pasin T, Ataoğlu S, Pasin Ö, Ankarali H. Comparison of the Effectiveness of Platelet-Rich Plasma, Corticosteroid, and Physical Therapy in Subacromial Impingement Syndrome. Arch Rheumatol. 2019 Mar 28;34(3):308-316. doi: 10.5606/ArchRheumatol.2019.7225. PMID: 31598597; PMCID: PMC6768781.
(31) Shams A, El-Sayed M, Gamal O, Ewes W. Subacromial injection of autologous platelet-rich plasma versus corticosteroid for the treatment of symptomatic partial rotator cuff tears. Eur J Orthop Surg Traumatol. 2016 Dec;26(8):837-842. doi: 10.1007/s00590-016-1826-3. Epub 2016 Aug 20. PMID: 27544678.
(32) Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med. 2013 Nov;41(11):2609-16. doi: 10.1177/0363546513496542. Epub 2013 Jul 26. PMID: 23893418.
(33) Cai YU, Sun Z, Liao B, Song Z, Xiao T, Zhu P. Sodium Hyaluronate and Platelet-Rich Plasma for Partial-Thickness Rotator Cuff Tears. Med Sci Sports Exerc. 2019;51(2):227-233. doi:10.1249/MSS.0000000000001781
(34) Lin J. Platelet-rich plasma injection in the treatment of frozen shoulder: A randomized controlled trial with 6-month follow-up . Int J Clin Pharmacol Ther. 2018 Aug;56(8):366-371. doi: 10.5414/CP203262. PMID: 29932415.
(35) Nejati P, Ghahremaninia A, Naderi F, Gharibzadeh S, Mazaherinezhad A. Treatment of Subacromial Impingement Syndrome: Platelet-Rich Plasma or Exercise Therapy? A Randomized Controlled Trial. Orthop J Sports Med. 2017 May 19;5(5):2325967117702366. doi: 10.1177/2325967117702366. PMID: 28567426; PMCID: PMC5439655.
(36) Pasin T, Ataoğlu S, Pasin Ö, Ankarali H. Comparison of the Effectiveness of Platelet-Rich Plasma, Corticosteroid, and Physical Therapy in Subacromial Impingement Syndrome. Arch Rheumatol. 2019 Mar 28;34(3):308-316. doi: 10.5606/ArchRheumatol.2019.7225. PMID: 31598597; PMCID: PMC6768781.
(37) Rha DW, Park GY, Kim YK, Kim MT, Lee SC. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil. 2013 Feb;27(2):113-22. doi: 10.1177/0269215512448388. Epub 2012 Oct 3. PMID: 23035005.
(38) Senna MK, Shaat RM, Ali AAA. Platelet-rich plasma in treatment of patients with idiopathic carpal tunnel syndrome. Clin Rheumatol. 2019 Dec;38(12):3643-3654. doi: 10.1007/s10067-019-04719-7. Epub 2019 Aug 16. PMID: 31420812.
(39) Pasin T, Ataoğlu S, Pasin Ö, Ankarali H. Comparison of the Effectiveness of Platelet-Rich Plasma, Corticosteroid, and Physical Therapy in Subacromial Impingement Syndrome. Arch Rheumatol. 2019 Mar 28;34(3):308-316. doi: 10.5606/ArchRheumatol.2019.7225. PMID: 31598597; PMCID: PMC6768781.
(40) Mishra AK, Skrepnik NV, Edwards SG, Jones GL, Sampson S, Vermillion DA, Ramsey ML, Karli DC, Rettig AC. Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med. 2014 Feb;42(2):463-71. doi: 10.1177/0363546513494359. Epub 2013 Jul 3. PMID: 23825183.
(41) Pasin T, Ataoğlu S, Pasin Ö, Ankarali H. Comparison of the Effectiveness of Platelet-Rich Plasma, Corticosteroid, and Physical Therapy in Subacromial Impingement Syndrome. Arch Rheumatol. 2019 Mar 28;34(3):308-316. doi: 10.5606/ArchRheumatol.2019.7225. PMID: 31598597; PMCID: PMC6768781.
(41) Martínez-Montiel O, Valencia-Martinez G, Blanco-Bucio P, Villalobos-Campuzano C. Tratamiento de epicondilitis de codo con plasma rico en plaquetas versus corticosteroide local [Treatment of elbow epicondylitis with platelet rich plasma versus local corticosteroids]. Acta Ortop Mex. 2015 May-Jun;29(3):155-8. Spanish. PMID: 26999966.
(43) Palacio EP, Schiavetti RR, Kanematsu M, Ikeda TM, Mizobuchi RR, Galbiatti JA. Effects of platelet-rich plasma on lateral epicondylitis of the elbow: prospective randomized controlled trial. Rev Bras Ortop. 2016 Jan 13;51(1):90-5. doi: 10.1016/j.rboe.2015.03.014. PMID: 26962506; PMCID: PMC4767828.
(44) Pasin T, Ataoğlu S, Pasin Ö, Ankarali H. Comparison of the Effectiveness of Platelet-Rich Plasma, Corticosteroid, and Physical Therapy in Subacromial Impingement Syndrome. Arch Rheumatol. 2019 Mar 28;34(3):308-316. doi: 10.5606/ArchRheumatol.2019.7225. PMID: 31598597; PMCID: PMC6768781.
(45) Gautam VK, Verma S, Batra S, Bhatnagar N, Arora S. Platelet-rich plasma versus corticosteroid injection for recalcitrant lateral epicondylitis: clinical and ultrasonographic evaluation. J Orthop Surg (Hong Kong). 2015 Apr;23(1):1-5. doi: 10.1177/230949901502300101. PMID: 25920633.
(46) Gosens T, Peerbooms JC, van Laar W, den Oudsten BL. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2011 Jun;39(6):1200-8. doi: 10.1177/0363546510397173. Epub 2011 Mar 21. PMID: 21422467.
(47) Merolla G, Dellabiancia F, Ricci A, Mussoni MP, Nucci S, Zanoli G, Paladini P, Porcellini G. Arthroscopic Debridement Versus Platelet-Rich Plasma Injection: A Prospective, Randomized, Comparative Study of Chronic Lateral Epicondylitis With a Nearly 2-Year Follow-Up. Arthroscopy. 2017 Jul;33(7):1320-1329. doi: 10.1016/j.arthro.2017.02.009. Epub 2017 Apr 19. PMID: 28433443.
(48) Raeissadat SA, Rayegani SM, Hassanabadi H, Rahimi R, Sedighipour L, Rostami K. Is Platelet-rich plasma superior to whole blood in the management of chronic tennis elbow: one year randomized clinical trial. BMC Sports Sci Med Rehabil. 2014 Mar 18;6:12. doi: 10.1186/2052-1847-6-12. PMID: 24635909; PMCID: PMC4006635.
(49) Thanasas C, Papadimitriou G, Charalambidis C, Paraskevopoulos I, Papanikolaou A. Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: a randomized controlled clinical trial. Am J Sports Med. 2011 Oct;39(10):2130-4. doi: 10.1177/0363546511417113. Epub 2011 Aug 2. PMID: 21813443.
(50) Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med. 2013 Nov;41(11):2609-16. doi: 10.1177/0363546513496542. Epub 2013 Jul 26. PMID: 23893418.
(51) Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med. 2013 Nov;41(11):2609-16. doi: 10.1177/0363546513496542. Epub 2013 Jul 26. PMID: 23893418.
(52) Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med. 2013 Nov;41(11):2609-16. doi: 10.1177/0363546513496542. Epub 2013 Jul 26. PMID: 23893418.
(53) Boesen AP, Hansen R, Boesen MI, Malliaras P, Langberg H. Effect of High-Volume Injection, Platelet-Rich Plasma, and Sham Treatment in Chronic Midportion Achilles Tendinopathy: A Randomized Double-Blinded Prospective Study. Am J Sports Med. 2017 Jul;45(9):2034-2043. doi: 10.1177/0363546517702862. Epub 2017 May 22. PMID: 28530451.
(54) Alsousou J, Thompson M, Harrison P, Willett K, Franklin S. Effect of platelet-rich plasma on healing tissues in acute ruptured Achilles tendon: a human immunohistochemistry study. Lancet. 2015 Feb 26;385 Suppl 1:S19. doi: 10.1016/S0140-6736(15)60334-8. PMID: 26312841.
(55) Solakoglu Ö, Heydecke G, Amiri N, Anitua E. The use of plasma rich in growth factors (PRGF) in guided tissue regeneration and guided bone regeneration. A review of histological, immunohistochemical, histomorphometrical, radiological and clinical results in humans. Ann Anat. 2020 Sep;231:151528. doi: 10.1016/j.aanat.2020.151528. Epub 2020 May 4. PMID: 32376297.
(56) Sánchez M, Fiz N, Azofra J, Usabiaga J, Aduriz Recalde E, Garcia Gutierrez A, Albillos J, Gárate R, Aguirre JJ, Padilla S, Orive G, Anitua E. A randomized clinical trial evaluating plasma rich in growth factors (PRGF-Endoret) versus hyaluronic acid in the short-term treatment of symptomatic knee osteoarthritis. Arthroscopy. 2012 Aug;28(8):1070-8. doi: 10.1016/j.arthro.2012.05.011. PMID: 22840987.
(57) Vaquerizo V, Plasencia MÁ, Arribas I, Seijas R, Padilla S, Orive G, Anitua E. Comparison of intra-articular injections of plasma rich in growth factors (PRGF-Endoret) versus Durolane hyaluronic acid in the treatment of patients with symptomatic osteoarthritis: a randomized controlled trial. Arthroscopy. 2013 Oct;29(10):1635-43. doi: 10.1016/j.arthro.2013.07.264. PMID: 24075613.
(58) Anitua E, Zalduendo MM, Prado R, Alkhraisat MH, Orive G. Morphogen and proinflammatory cytokine release kinetics from PRGF-Endoret fibrin scaffolds: evaluation of the effect of leukocyte inclusion. J Biomed Mater Res A. 2015 Mar;103(3):1011-20. doi: 10.1002/jbm.a.35244. Epub 2014 Jun 12. PMID: 24890049.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
