What is the Ligamentum Flavum? Why Should You Care?

Credit: Shutterstock
One of the more critical ligaments in your spine is generally an unknown for most patients. That’s despite being responsible for causing lots of back pain and general havoc. That structure is called the ligamentum flavum. Let’s dig in.
Ligaments and the Spine
If we had to hold a competition between different spinal structures like discs, vertebra (spinal bones), nerves, muscles, facet joints, and ligaments-you could make a credible argument that the ligaments are some of the most important structures. However, when’s the last time you read an MRI report that even commented on the status of the ligaments? You see lots of things talked about in those reports like disc bulges, facet joints, nerves, etc… Ligaments just usually don’t make the list. Why?
Before we get deeper into this topic, take a few minutes and watch my video about how the parts and pieces of the spine come together:
I often say that ligaments are the red-headed stepchild of the spine. 99% of physicians that interact with back or neck pain seem to ignore them, yet when it comes to preventing instability (things moving around too much causing pain), ligaments are the key player. Strong ligaments prevent abnormal movement and protect the spine. Weakened or damaged ligaments cause instability and that leads to degenerative disc disease and often pain.
One of the ligaments you can see commented about on an MRI report is the ligamentum flavum. This one is critical when a patient has central canal stenosis. Let’s dive into what that is and why it’s so important.
The Ligamentum Flavum
In medicine, like law, we physicians love to use Latin. Why? It makes sure we can use big words that patients won’t understand. Such is the case with the term, “ligamentum flavum”. That bit of ancient Greek and Roman Latin means “yellow ligament”. Now we could just say yellow ligament and that would be easier, but then you would know what we’re talking about!
This ligament is in fact yellow and lives in the very back of the spinal canal. Before we get into what it does, you may want to watch the video above if you haven’t done that yet. For example, it’s important to know that the spinal canal is where the spinal cord and spinal nerves live and is created by the holes in the vertebrae that stack one on the other. This is a diagram I created:
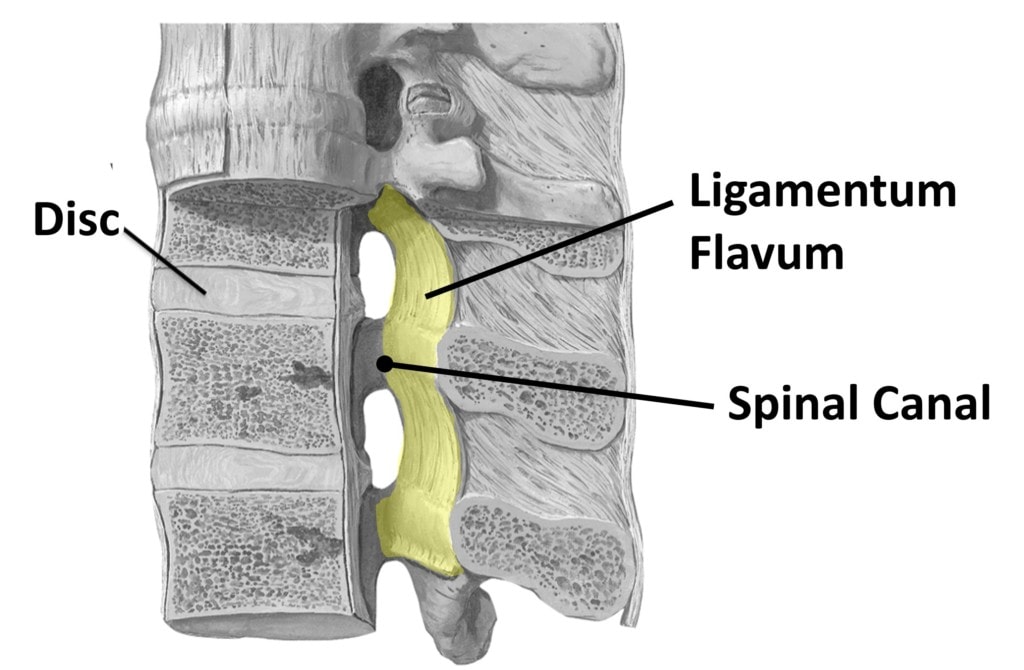
I colored the ligamentum flavum here yellow. It goes from vertebra to vertebra in the backmost part of the spinal canal. What’s its purpose? Like all ligaments, it helps allow motion between the vertebrae while also keeping them aligned. This one is stretchy, so it permits flexion or bending forward.
Central Canal Stenosis
In medicine, the word stenosis means less room in a canal where something traverses. That could be an artery or a vein or in the spine, the term usually refers to the spinal or foraminal canals. Here we’re discussing the main spinal canal that goes up and down through the vertebrae, also called the “central canal”.
In central canal stenosis, this area gets too small. We’ll discuss this area in terms of the low back today, as it’s often easier to see the structures in that area. In this case, there are a number of structures that can impinge on this canal and make it smaller:
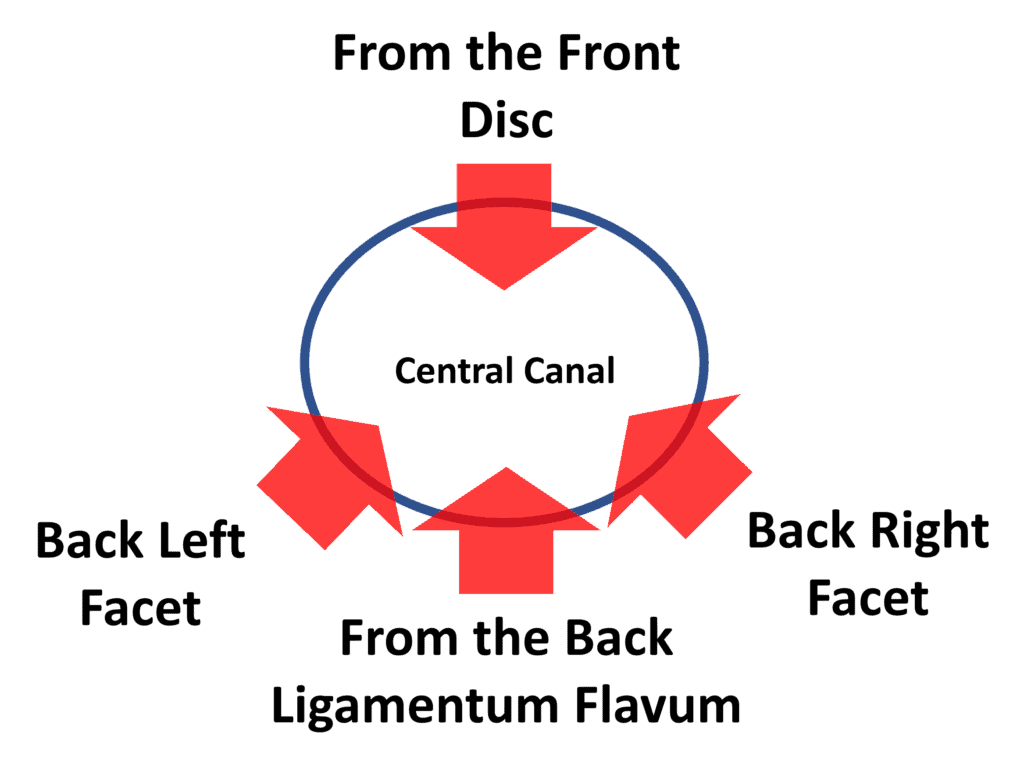
As you can see, the disc bulging from the front or the facet joints from the backside (also called facet hypertrophy) can make the spinal canal stenotic (smaller). In the same way, the ligamentum flavum from the backside can get bigger and cause the canal to be smaller as well.
Ligamentum Flavum Hypertrophy
All ligaments or tendons that get overworked and can’t completely heal themselves get bigger, which in medicine we call hypertrophy. That happens because a dense ligament is young and strong, but when your body can no longer completely heal the ligament, it keeps throwing new weaker tissue at the area. On the one hand, more weak tissue reduces the likelihood that the ligament will ultimately fail and tear, but on the other, that ligament now takes up much more space.
The ligamentum flavum also hypertrophies, usually because of degenerative instability. That means it gets beat up by the extra movement between the vertebra caused by loose ligaments and disc collapse. Now ordinarily that wouldn’t be a problem but remember this ligament lives in the spinal canal and the spinal nerves run through that canal. Hence a smaller canal means that these nerves get crunched:
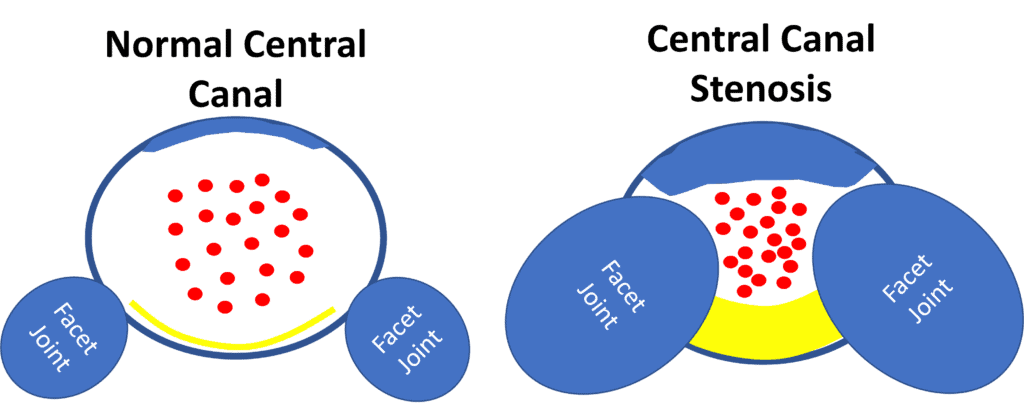
On the left, you see the normal central canal with the disc in the front (top of this image), the smaller facet joints in the back part, and then the dense and thin ligamentum flavum (yellow line). On the right you see a stenotic central canal with a disc bulge up top, enlarged and arthritic facet joints, and a thicker and hypertrophied ligamentum flavum. The red dots in both diagrams represent the spinal nerves going through the canal. As you can see, they get crunched in the middle when stenosis is present. When spinal nerves lack room, they tend to get very upset and irritated, leading to back pain, numbness, and tingling or weakness in the legs or feet.
What Happens to the Ligamentum Flavum as You Move?
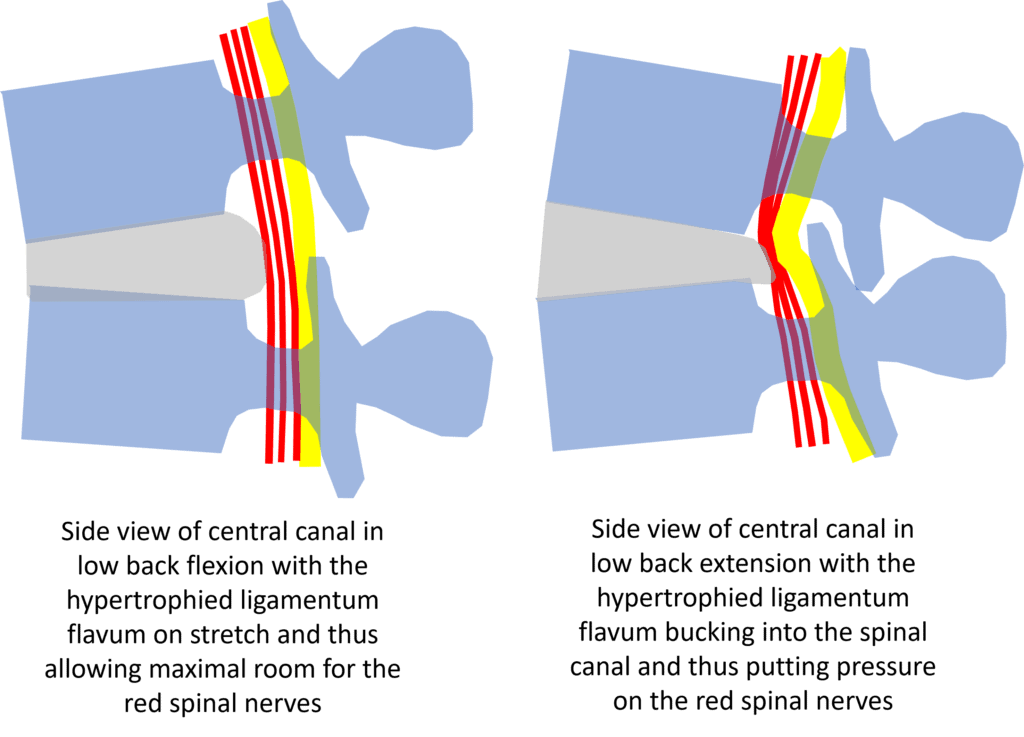
Patients with central canal stenosis due to an enlarged ligamentum flavum love low back flexion. In fact, there’s something called a “shopping cart sign” where they can walk through a grocery store without pain or leg symptoms as long as they lean forward a bit on a shopping cart. Why?
In my diagram above, this is now the side view (rather than the top-down view shown above). Note that the yellow ligamentum flavum is on stretch when the low back is in flexion and thus allows the red spinal nerves lots of room. However, when the patient stands up straight or extends, note that the yellow ligamentum flavum now buckles into the spinal canal. This compresses the red spinal nerves against the disc bulge. This is why standing for any length of time or worse, going downhill on a hike, quickly causes back pain and/or leg symptoms in patients with central canal stenosis.
How Do You Fix This?
The traditional way that central canal stenosis has been handled has been surgical. Basically, a big back surgery (wide laminectomy/discectomy) to open up the canal by taking out the disc bulge, removing the inside of the facet bones and lamina (back of the spinal canal), and then cutting out the ligamentum flavum. While this generally works to allow more room for the spinal nerves and reduce symptoms, removing all of that stuff often leads to more instability. That can then lead to the disc bulging again and the facets getting more arthritis and the cycle repeats. Because of that problem, surgeons these days often add a fusion, which is where the spine is bolted together. However, that can then lead to the adjacent segments above and below getting too much wear and tear and breaking down (called adjacent segment disease). To learn more about that issue, see my video below:
Can This Problem Be Helped Without Surgery?
In my video above, I describe the interventional orthobiologics procedure we use to help central canal stenosis and degenerative disc disease. In addition to injecting your platelet-based products into the ligaments, around nerves (epidural), into arthritic facts, and into atrophied muscles, we can also directly inject the ligamentum flavum. Why? the goal is to get it smaller and denser by promoting repair within the ligament. We don’t need a huge amount of room, just a few millimeters less buckling when the person stands, and that can make a huge difference in standing and walking tolerance. For example, in my clinical experience, we can usually get patients from non-functional 5-15 minutes standing time (before they need to sit due to pain) to a functional 1-2 hours.
The upshot? Now you know about the yellow ligament that lives in the back of the spinal canal that can cause so much misery for so many people. Our first goal should always be to keep the ligaments and all of your other critical parts and pieces and thus avoid surgery. We can usually do that with our platelet-based DDD procedure!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
