What My Unstable Knee Can Teach You About PRP Treatment

Credit: Shutterstock
I’ve blogged about my right knee which is a case study in Instability and why a PRP injection MUST include more than injecting inside the knee joint. Let’s review the concept of Instability and why it’s so critical for doctors who use PRP to understand this issue. Let’s dig in.
The Knee
Credit: Shutterstock
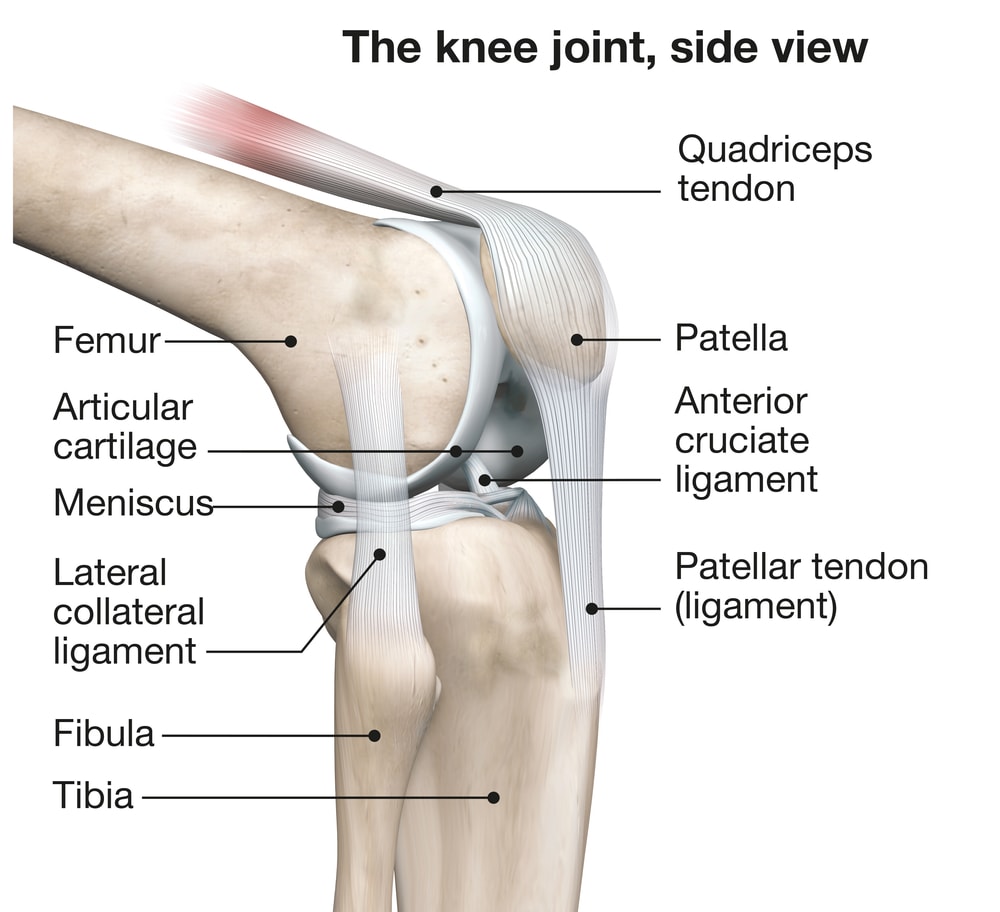
Your knee is made up of two bones that meet (the Femur and the Tibia) and your knee cap, which are all lined with cartilage. There’s a Meniscus that acts as a shock absorber as well as a slew of ligaments. Those ligaments, when completely torn are often a focus of knee surgery. However, when those ligaments are loose, they’re often ignored like a red-headed stepchild.
Ligament Subfailure
Ligaments can be torn in half, but MUCH more commonly they get irreversibly stretched and become lax. Both of these things cause instability or a joint that gets beat up way too much as it moves because of abnormal motion. This latter type of Instability, which I call “ligament sub failure” is missed about 99% of the time by Orthopedic surgeons. The exam skills to diagnose it just aren’t there because their exam is focused on whether a ligament should be operated.
In my clinical experience, ligament sub failure is the most common cause of Arthritis. Hence, the fact that it’s almost always missed is a huge public health problem. Let’s explore this concept a bit through my knee.
My Right Knee
Several years ago I was at our licensed Cayman Island site on the weekend and I jumped out of a boat into what I thought was 10+ feet of water. Regrettably, it turned out to be much shallower and my right knee forcefully and unexpectedly hit the bottom at a strange angle. That knee blew up by that evening and ever since then has been an on and off problem. Initially, I got a few high-dose PRP injections inside the joint, which helped. However, last year I was sitting and simply went to get up and felt pain in the knee. After several days of swelling, once it claimed down again, I began to notice that how my knee was positioned when sitting would determine if I would get another episode. The knee also felt “loose”. It was at that point that I knew that I had an Instability problem.
How Do You Diagnose Sub Failure Instability in a Knee?
I recently had one of our Fellows perform an exam on my knee using a stress ultrasound. This is where the Doctor uses Ultrasound to image the ligament (and Meniscus if it’s a Collateral ligament) and then physically stresses that side. The ligament should hold everything tight. However, if the doctor sees movement in the bones and ligament (and/or Meniscus) that knee is unstable with a loose ligament. For example, here’s an Ultrasound of the bones and Meniscus moving when stressed:
Again, in the video, if the knee was normal, nothing should move.
If you’ve been to see a Doctor about your knee and this test using Ultrasound and stressing the knee was never performed, then you didn’t get a complete exam. You may have Sub Failure Instability and not know it, which is a VERY bad place to be.
PRP Treatment for Arthritis vs Arthritis + Instability is Completely Different
In Arthritis without Instability, injecting high-dose PRP into the knee joint can be very effective. However, when we add in loose ligaments causing Instability, what needs to be injected to get the best result changes drastically. Now the provider has to have the expertise to inject the loose ligaments with PRP as well. That’s easier said than done in most clinics.
First, to figure out which ligaments to inject, you have to understand how to detect Sub Failure Instability. As I’ve said, 99% of Physicians have never been trained in this kind of exam. Second, you need to know how to use precise imaging guidance to place PRP into the damaged ligaments. This means using BOTH Ultrasound AND Fluoroscopy (real-time x-ray imaging).
Let’s review a little bit about the tools needed to inject all of the ligaments in the knee.
Ultrasound + Fluoro Are Essential for a Complete Ligament Treatment of the Knee
While some Physicians have begun to add Ultrasound imaging to help with more precise knee injections, it takes more than that to treat an unstable knee. Why? Let’s dive into that subject.
Ultrasound is great for helping precisely injecting something inside the capsule of the knee joint (intra-articular). It’s also great for injecting superficial ligaments like the Medial or Lateral Collateral ligaments. Where it often fails is in injecting the deep ligaments of the knee like ACL and PCL. That’s because these ligaments are often shrouded by bone, so the Ultrasound signal can’t bounce in and out well enough to create an image of all parts of these structures. I’ve created a video on this problem with the ACL if you want to learn more:
To inject these deep ligaments in most patients, you need Fluoroscopy, which is a real-time x-ray. However, that creates big issues for many Physicians. Why? First, Fluoroscopy will cost 3-4X what an Ultrasound setup runs. That’s because of the fact that the machine is more expensive, that machine has to be run by a Rad tech, and the room in which it’s used has to be much bigger with specialized walls. However, there’s another problem often faced by employed Physicians who work for a hospital or in an Academic Medical Center. In that case, the only place that Fluoroscopy machines exist are in an Operating room or Ambulatory Surgery Center, and getting access to them is either prohibitively expensive or impossible.
How do you solve that last issue? For example, at our Colorado HQ site, we have created multiple procedure rooms in the office. We also employ multiple Rad techs and have three Fluoro machines ready to use when needed.
Getting Back to My Knee
My knee needed the MCL ligament on the inside and ACL injected. Hence, I had Dr. Markle inject my joint as well as these two ligaments with high-dose PRP. He injected the MCL with Ultrasound and the ACL with Fluoroscopy. The result? My knee now feels stable and no longer feels loose. It no longer “gets out of place” when I sit, because the loose ligaments allowing that movement have been tightened down by the injections. It also no longer routinely swells after workouts because it’s not getting beat up when I work out.
The upshot? At the end of the day, understanding that Sub Failure Ligament injuries are common could help save the US healthcare system billions in knee replacements and other surgeries. To do that we need to educate armies of Physicians on how to detect the problem and then outfit thousands of offices with the tools to be able to precisely inject these ligaments! I for one am glad I recognized my issue early and had our experts treat it!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
