Which Ligament Allows for Excessive C1-C2 Overhang?
This blog is specific to the topic of upper cervical instability. In that patient population, we often get a Digital Motion X-ray open mouth view looking for sideways motion of C1 on C2 (aka “overhang”). When we see that, which ligament is responsible for allowing that to happen? Let’s dig in.
The Upper Cervical Ligaments
First, I wrote a whole book on this topic, so if you want to learn more about craniocervical instability or when the ligaments that hold the head on are loose, click on the book cover below:
Below are some of the main ligaments that hold the head onto the spine. Note the alar ligaments come from what’s called the dens of C2 (solid blue) and reach up and connect to the skull.
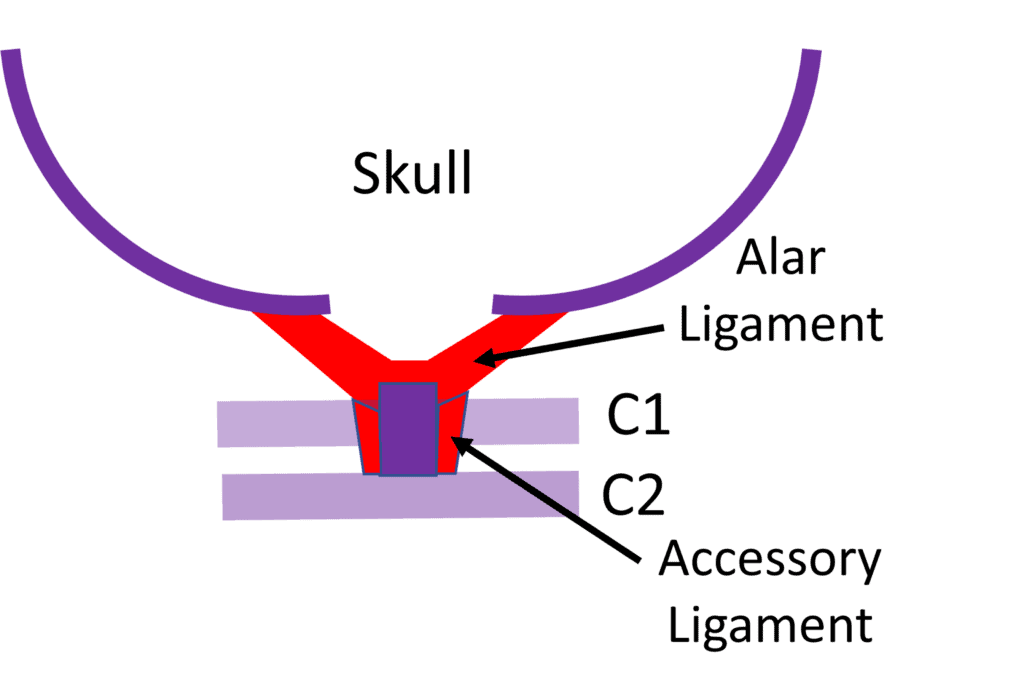
Today we’ll focus on those alar ligaments.
C1-C2 Overhang and CCI
CCI means craniocervical instability. That’s instability from C0-C2 (sometimes C2-C3 is thrown in as well). The symptoms are headaches, dizziness/imbalance, neck pain, brain fog, and lots of other things. The cause is usually head and neck trauma, but can also be congenitally loose ligaments or a condition called Ehlers-Danlos syndrome.

Photo by Paul Aiken / The Camera
While there are several different ways to find CCI on imaging, a popular one that now has some of the best research support out there is called Digital Motion X-ray or DMX. That’s a machine that takes a live video of the upper neck bones as the patient moves. The goal is to find areas of excessive motion due to damaged or loose ligaments.
Recently published research showed that when there was asymmetry of the dens in the atlas, then the following overhang measurements corresponded to the chances of the patient being correctly classified into the “traumatic” versus normal category (1):
- 2-3 mm overhang – 67%
- 3+ mm overhang – 95%
Realize that studies like this comparing normal to traumatically injured patients have not been done for many commonly used neurosurgical measurements that are believed to indicate CCI. That makes DMX one of the best-researched methods to detect CCI.
What the Heck is C1-C2 Overhang?
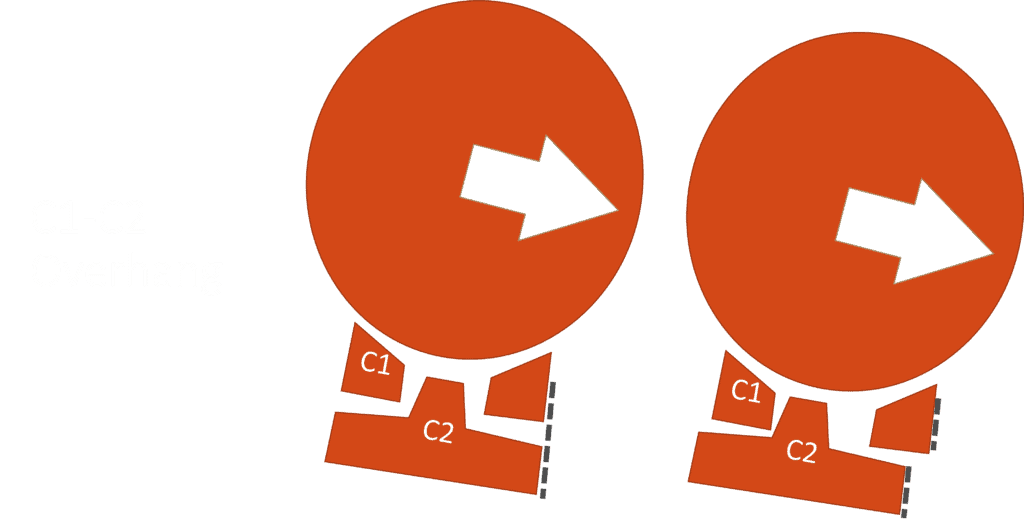
When you bend your head sideways, the alar ligament helps to keep C1 stable against C2. That means that the corners of the two bones as shown on the left above stay aligned (dashed lines). However, when there is C1-C2 instability as shown on the right, the corners don’t line up. Here C1 has shifted laterally relative to C2.
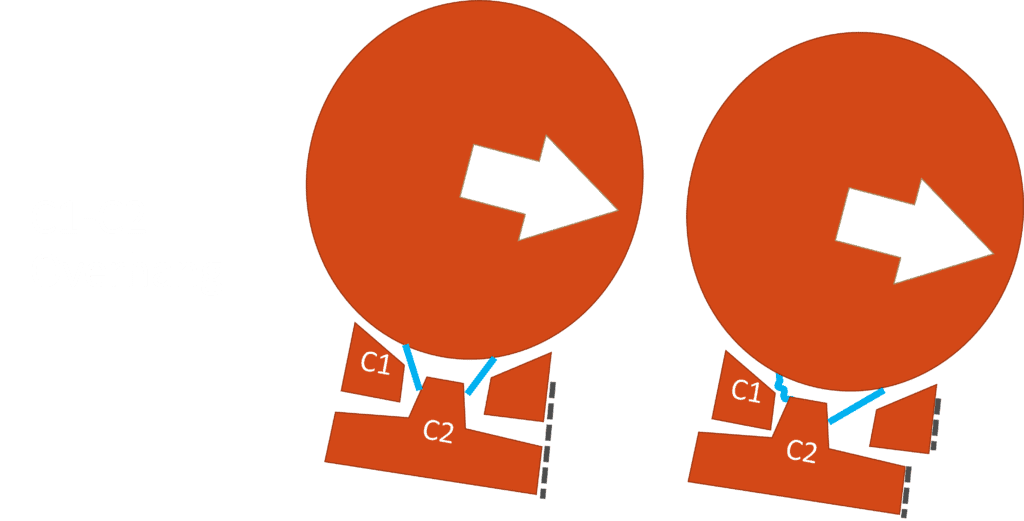
So which alar ligament would allow this motion? Above I drew in the alar ligaments as light blue lines. When the shift occurs on the right above, it’s the same side alar ligament that’s stretched to allow that movement. That assumes that the skull (C0) and the atlas (C1) are moving together (which is common). The other side is lax.
Hence the alar ligament on the side of the overhang is the culprit that allows the extra motion to occur.
Why Would We Care?
If a surgeon is just going to fuse C1-C2 together with a screw, then this thought exercise is unimportant. However, that’s a huge surgery with a high serious complication rate that also eliminates 50% of all cervical rotation (which usually occurs at C1-C2). That surgery also sets the patient up for the C0-C1 and C2-C3 segments to rapidly wear out through adjacent segment disease, requiring more surgeries. That’s because all of that force that was handled by C1-C2 now gets shunted to the levels above and below.
However, if we can help the damaged alar ligament heal through a precise injection, now which one is damaged becomes important because that ligament may need more attention. To accomplish that without a big surgery, I created the PICL procedure (Percutaneous Implantation of the Craniocervical Ligaments), which uses dual-axis c-arm fluoroscopy, endoscopy, and a 3-D printed mouthpiece to target the damaged alar ligament (or both if needed).
A Case Study
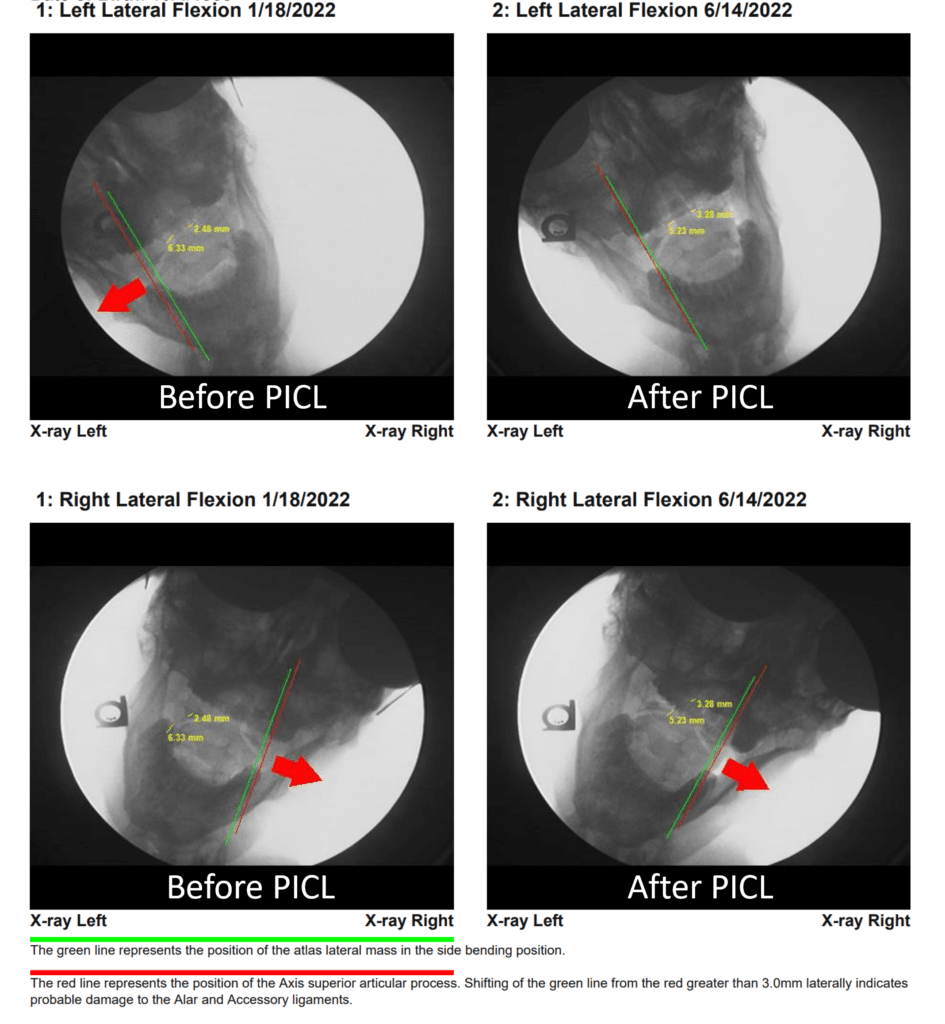
Above, you see the DMX images measuring overhang in a real patient who underwent a first PICL procedure. On the left lateral flexion view from 1/18/22 (left above) labeled “Before PICL” you see the two lines that measure the amount of C1-C2 overhang. They are apart, so they measure a moderate amount of C1-C2 overhang. On the Left Lateral Flexion 6/14/2022 labeled “After PICL” (right above) you see that those same two lines are now together, indicating that there is no longer a C1-C2 overhang to that side. In the bottom two images (Right Lateral Flexion 1/18/22 and 6/14/22), there is no change in the separation of the lines from before and after the first PICL procedure, so no change in the overhang on that side. Hence, this patient now has a normal overhang on the left after the first PICL procedure and still has an abnormal overhang on the right. Hence, we can now use this data to make sure the second PICL procedure really focuses on getting the alar ligament on the side of the overhang.
The upshot? Knowing which ligaments allow for which kind of excessive movement is often critical in using advanced interventional orthobiologics to help the patient recover. In the case of CCI, that’s understanding which alar ligament causes the overhang!
___________________________________________________
References:
(1) Freeman MD, Katz EA, Rosa SL, Gatterman BG, Strömmer EMF, Leith WM. Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma. Int J Environ Res Public Health. 2020 Mar 5;17(5):1693. doi: 10.3390/ijerph17051693. PMID: 32150926; PMCID: PMC7084423.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.