Which Regenexx Procedures Fail the Most?
Credit: Shutterstock
In the Wild West of stem cells, most of what you see are either fictional outcomes that are really customer satisfaction surveys or testimonials by social media influencers. One thing you never see is anything like today’s blog where a company offering orthobiologic treatments discusses its failures. So let’s dig into this topic.
Real Procedures Have Success and Failure Rates
As any physician can tell you, any procedure ever used in medicine has a success and failure rate. Yet, this reality is suspended in the marketing of stem cell procedures. Many times you see customer satisfaction data with crazy high percentages of success. Other times testimonials. In a few instances, you see something that looks like a success rate, but that’s not generally from all consented and treated patients. Hence, the success and failure rates of procedures remain largely unknown. Why? To know that, you have to track a large chunk of the treated patients over time in a registry.
What Is a Registry?
A registry is a system where patients are tracked over time. When the patient is treated, they’re entered into a registry, and before the procedure, they fill out validated questionnaires. Then at set time points, they’re pinged with the same questionnaires. This generates data that can be tracked, analyzed, and reported to improve care and inform patients how likely they are to have a good outcome. In addition, the registry data can help decide which patients are good or bad candidates for the specific procedure being tracked.
Regenexx has the world’s largest and oldest orthobiologics registry. There isn’t even a distant second. While many academics in orthopedics have been calling for everyone to use registries and there are companies out there starting to collect data, so far, we’ve been the only company whose registry is old enough to be a junior in high school (16 years)! All other registries tracking this data are still in preschool.
Surgical Conversion Rates
For a procedure that exists to help patients avoid surgery, the single most important data point is how many patients convert to surgery despite having a procedure. Hence, we have been tracking these conversion rates for years. Below you see six different joints where we have reported these rates for different body areas. These screens are from our Registry Insights Tool that any provider on the network can access:

The red in the bars off to the left represent the percentages of patients that converted to surgery at each time point. Meaning at 1, 3, 6,12 months, and 2, 3, and 4 years after the procedure. The circles off to the right represent the types of procedures to which they converted. The joint procedures shown were bone marrow concentrate procedures and for the neck and back procedures shown, these were primarily platelet-based procedures. So for example, 7.1% of knee arthritis patients treated with bone marrow concentrate converted to knee surgery by 48 months, with the most common procedure being a knee replacement.
What Does All of This Mean?
Out of tens of thousands of patients tracked in the registry, few report converting to surgery. That’s a great thing. However, what can we learn by digging into this data?
First, how should we view these individual numbers? Meaning, the numbers reported at each time point could be additive. So when someone reports at 2-years that they had surgery, the same person likely won’t respond to their 3-year survey. Or they could be repetitive. Meaning that the person may still answer a survey telling us a second time that they had surgery. For this discussion, we’ll consider the absolute worst, that every patient who responded that they got surgery dropped out and never responded again. This means we’ll add all of the numbers together to get a final surgical conversion rate, which is likely a significant overestimate of the number of patients who actually got surgery despite a treatment.
If we add up all of the patients reporting that they converted to surgery by 48 months after a knee bone marrow concentrate procedure, it’s about 22% by 4 years or roughly 1 in 5. Given that most of those patients are knee replacement candidates at the time of the procedure, that’s pretty darn good and that’s roughly consistent with other sampling surveys we’ve done through the years via phone calls which peg this rate at 10-20%.
If we look at the low back, the percentage of patients out to 4 years that convert to lumbar fusion 4 years after a platelet-based procedure is about 8%. For shoulder, the percentage that converts to a shoulder surgery four years after a bone marrow concentrate procedure is about 18%. That’s in the context of about half of these patients needing shoulder replacement and the other half needing rotator cuff repair.
Hips Are Tough
If we look at the hip patients above, we see quite a bit more red in the bars to the left. If we take the sum of all of the percentages at all of time points for each treated joint, we get this graph:
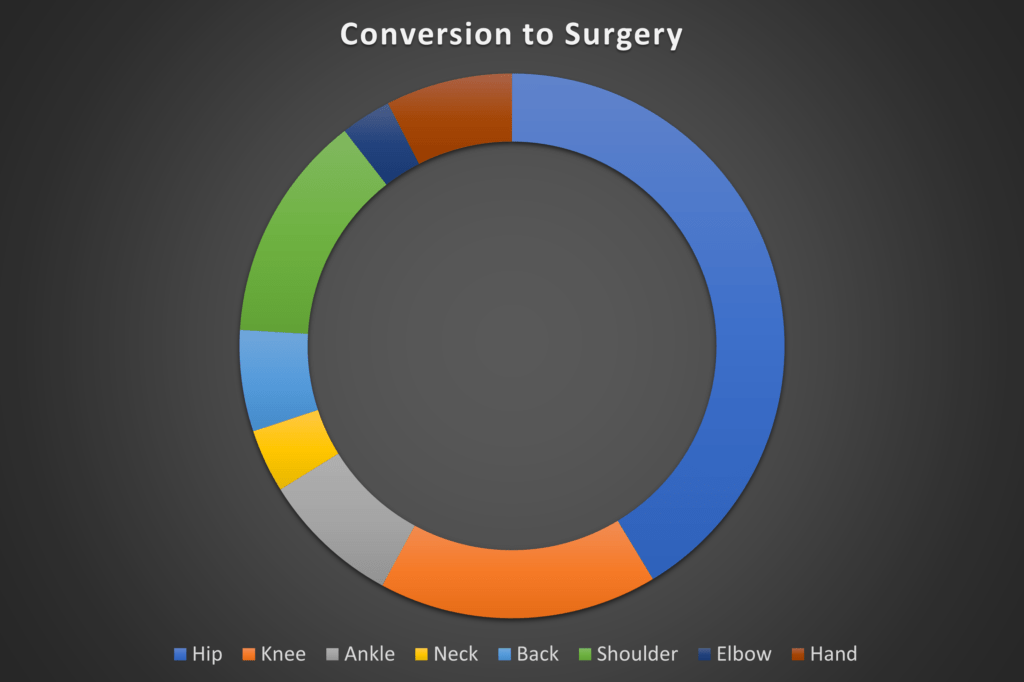
Hip injection patients are 3 times more likely to convert to surgery. This has been a consistent issue in our data for more than a decade and a half.
Why are hips are converting to surgery at a greater rate? Based on our research, if you have severe hip arthritis (which is about half the hips we see in the office), you are highly likely to convert to a hip replacement despite the procedure we offer. Patients with mild to moderate hip arthritis or just labral tears fare better. In contrast, this is NOT the case with knee arthritis. In this joint, patients with severe arthritis do very well, hence the difference in the data above.
This phenomenon of hips being harder to repair than knees has also been discussed from a scientific standpoint. For example, we know that the progenitor cells in hip joints are less likely to be able to repair than those found in knees (1). We also know that the extra-cellular matrix in hips is chronologically much older than in knees and is, therefore, less able to be able to heal cumulative damage (2).
Why Tell You Any of This?
If I wanted to maximize income for Regenexx, I wouldn’t be sharing any of this. In fact, I also wouldn’t have a registry at all. I would just find a few patients that responded well to a hip procedure and broadcast that everywhere I could. I would also find a cadre of social media influencers with hip problems and treat them all for free and then pay those that did well to recruit their followers to get hip procedures. However, that’s not how we roll.
Analyzing Registry Data
Having a registry is ridiculously expensive. Herding the physician cats to make sure they get surveys to patients before they get their procedure is hard work. In fact, my medical director dashboard just showed that I needed to remind several clinics to do a better job of that. Finally, analyzing this data takes hundred of hours.
For example, this past year we looked at the shoulder arthritis data. We did find two things that predicted a poorer prognosis after reviewing a huge number of MRIs and having one of our data scientists work that dataset. Ultimately, we didn’t publish those findings and decided to keep that in-house for our Regenexx providers. Meaning only they have access to that data to decide which shoulder patients should be placed into the “poor candidate” category.
We’ve also looked at knee and hip candidacy data many times through the years and are now looking at this again. We’ll have that most recent data analysis done by the end of the year. The goal here is to find one or two hints on MRI that will allow our providers to determine which patients are the most likely to convert to surgery. For hips, we already know that severe disease is bad. For knees, so far everything is a green light, but that can always change based on subsequent data analysis.
The upshot? We collect and transparently report our data because that’s what real medical providers do. They continually look at the data to see what’s working and what’s not working and make sure that everyone knows that information so they can make informed decisions. Regrettably, right now, nobody else but Regenexx has enough data to do that, but we hope we see more providers join the registry and data reporting club! For example, we know that several companies have formed to offer this service to doctors, which we see as a net positive for the field!
________________________________________________
(1) Catterall JB, Hsueh MF, Stabler TV, et al. Protein modification by deamidation indicates variations in joint extracellular matrix turnover. J Biol Chem. 2012;287(7):4640-4651. doi:10.1074/jbc.M111.249649
(2) Maroudas A, Bayliss MT, Uchitel-Kaushansky N, Schneiderman R, Gilav E. Aggrecan turnover in human articular cartilage: use of aspartic acid racemization as a marker of molecular age. Arch Biochem Biophys. 1998 Feb 1;350(1):61-71. doi: 10.1006/abbi.1997.0492. PMID: 9466821.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
