Whiplash Leads to More Long-term Pain at 20 Years
Does getting a neck injury in a car crash, even if it heals, cause long-term problems? That’s what a recent study set out to determine. Let’s dig in.
WAD
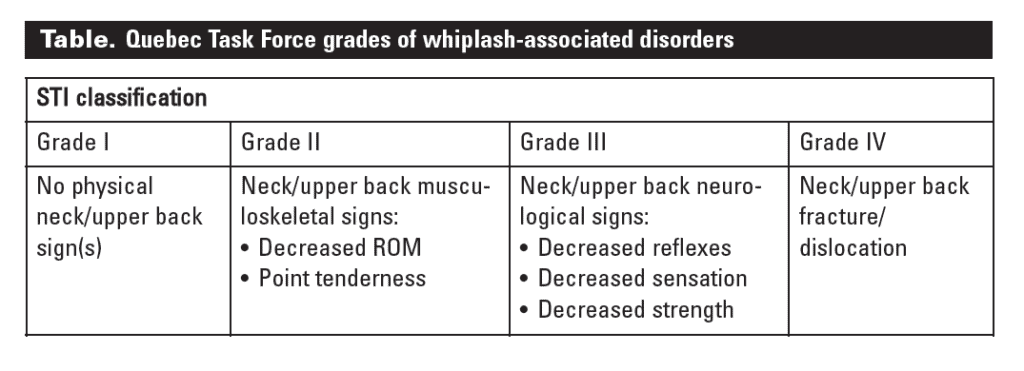
More than 20 years ago, some Canadian researchers in Quebec (QTF or Quebec Task Force) came up with the term “WAD” which means “Whiplash Associated Disorders” (1). Some of them infamously later claimed that WAD 1 or 2 (neck pain after a car crash) could never produce long-term pain and that the patients who had those issues were making it up or had psychological problems (2). Much of that was based on the fact that few of these patients had the traditional MRI findings like a herniated disc that required surgery. Our research group, many years ago, refuted this idea (3).
Shortly after that, the world of diagnosing neck pain after a car crash grew up and the idea that you could treat both pain and psychological distress by treating injured facet joints matured. Since then, the concept that some of these patients also have injuries to critical neck ligaments became a thing, especially as regenerative therapies came to the forefront. Hence, for real physicians here in the satates, the WAD house of cards as first created by the QTF just became irrelevant over time. However, not so for most Canadians, who are still forced to deal with the long-term effects of QTF.
Do Acute Whiplash Patients Have Long-term Pain?
Today we’ll review a new study that hopefully puts the final stake through the heart of QTF (4). How does that work? Let’s dig in.
Between 1993 and 1996, Japanese researchers found 508 acute whiplash patients and 497 asymptomatic volunteers, all of whom underwent neck MRI and physical examinations. For this 20-year follow-up, they recontatced 75 of the whiplash patients and 181 of the control subjects. They also compared MRI findings at 20 years between the groups.
What did they find? Shoulder stiffness was nearly twice as prevalent in the whiplash group (72.0% vs. 45.9%), headache was more than twice as common (24.0% vs. 12.2%), and arm pain was >4X more common (13.3% vs. 3.9%). The odds of having these symptoms two decades later once other factors were removed were even higher (shoulder stiffness (odds ratio [OR]: 3.36), headache (OR: 2.39), and arm pain (OR: 3.82)).
Of note, there were no worse MRI findings in the whiplash group at 20 years, continuing to defy the concept that it needs to be on an MRI report to be real.
The Green Poultice?
Some of the original Quebec Task Force members who came up with this grading scale were convinced that patients with neck injuries who didn’t need surgery and who developed long-term pain neck pain were exaggerating their symptoms for financial gain. However, this 20-year follow-up stated:
“No patients had been involved in litigation, and they had received no financial compensation at the 20-year follow-up.”
In addition, this paper used acute whiplash and not chronic patients. These people, when identified, had not considered their neck pain as any kind of disability. They were merely exposed to a crash and had acute neck pain. Meaning that these were not people who at the time of their recruitment were receiving emotional gain from being chronically injured.
What’s Causing These Injuries?
So what can cause people to have more shoulder issues, headache, or arm pain 20 years later? Here’s a shortlist:
- Neck facet joint injury
- Damaged ligaments
- Injured nerves
All of these things don’t show up well on MRI.
The upshot? A whiplash injury can cause pain for decades. We have treated several thousand whiplash-related neck injuries with precise orthobiologic injections and can usually help! In the meantime, I’m so glad that the crazy attempt by the Canadian government to pretend that people with injured necks had no real problems is finally dead once and for all!
________________________________________________
References:
(1) Sommer HM. Quebec Task Force’s scientific monograph on Whiplash-Associated Disorders (WAD). Spine (Phila Pa 1976). 1997 Apr 15;22(8):928. doi: 10.1097/00007632-199704150-00024. PMID: 9127933.
(2) Ferrari R, Kwan O, Russell AS, Pearce JM, Schrader H. The best approach to the problem of whiplash? One ticket to Lithuania, please. Clin Exp Rheumatol. 1999 May-Jun;17(3):321-6. PMID: 10410265.
(3) Centeno CJ, Freeman M, Elkins WL. A review of the literature refuting the concept of minor impact soft tissue injury. Pain Res Manag. 2005 Summer;10(2):71-4. doi: 10.1155/2005/536476. PMID: 15915248.
(4) Watanabe K, Daimon K, Fujiwara H, Nishiwaki Y, Okada E, Nojiri K, Watanabe M, Katoh H, Shimizu K, Ishihama H, Fujita N, Ichihara D, Tsuji T, Nakamura M, Matsumoto M. The Long-term Impact of Whiplash Injuries on Patient Symptoms and the Associated Degenerative Changes Detected Using MRI: A Prospective 20-year Follow-up Study Comparing Patients with Whiplash-associated Disorders with Asymptomatic Subjects. Spine (Phila Pa 1976). 2021 Jun 1;46(11):710-716. doi: 10.1097/BRS.0000000000003901. PMID: 33394988.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
