Why Are Physicians Addicted to Steroids? Tendons and Windex
Physicians have a torrid love affair ongoing with a medication that clearly harms their patients, but they just can’t seem to give it up. That medication can chew up joint cartilage and damage tissues, but they continue to inject it with wild abandon. That nasty drug fits into a class called corticosteroids. Let’s explore this bizarre and dangerous addiction through yet more studies on tendons that shows just how bad this tryst is for both parties.
What Is Addiction?
This is the Marriam-Webster definition:
- : a compulsive, chronic, physiological or psychological need for a habit-forming substance, behavior, or activity having harmful physical, psychological, or social effects and typically causing well-defined symptoms (such as anxiety, irritability, tremors, or nausea) upon withdrawal or abstinence : the state of being addicted
- : a strong inclination to do, use, or indulge in something repeatedly
Corticosteroids
If you remember the movie “My Big Fat Greek Wedding”, the father believed that Windex cured everything from eczema to poison ivy and everything else in-between. Today’s physicians use corticosteroid drugs in much the same way as the crazy father spraying Windex on everything. You got pain? You need a steroid shot. Inflammation? Steroid shot. Lack of motion? Steroid shot. Arthritis? Steroids! A torn tendon? More steroids.
Corticosteroids are old drugs, with the first one hitting the market in the 1940s (1). They are a group of hormones produced in the adrenal gland that both exist in the body in minuscule nanogram doses (a billionth of a gram) and are made synthetically as drugs in massive milligram doses (one million times more concentrated). The problem with the drug versions of these hormones is the dose difference that I’ll discuss below.
What are the common corticosteroid drugs? A long time ago, there was a drug called “cortisone”. That drug became so popular, that just like the term “Band-Aid” the term is still widely used today to describe the whole drug class. Actual corticosteroid drug names include:
- Bethamethasone, (Celestone)
- Prednisone
- Prednisolone
- Priamcinolone (Aristospan and Kenalog)
- Methylprednisolone (Medrol, Depo-Medrol, and Solu-Medrol)
- Dexamethasone
The Side Effects Are Worse than Windex
These are nasty drugs when it comes to side effects. Those include:
- Elevated blood sugar
- Osteonecrosis (bone that turns to mush)
- Increased risk of infection
- Glaucoma
- Fluid retention
- High blood pressure
- Confusion or delirium
- Weight gain and cushingoid syndrome (bizarre fatty deposits like a moon face)
- Osteoporosis
- Suppression of adrenal gland hormone production
The big problem for patients in pain is that they have been shown to make arthritis worse, increase the rate of infections if a joint replacement is later required, and to cause osteoporosis in women when injected epidural.
Research on Tendons
The idea that steroid shots can hurt tendons is not new. We’ve seen several studies that show that these injections wreak havoc in tendons. For example, we know that steroids injected into elbow tendons actually make tennis elbow pain worse in the long-run (2). To add fuel to the Windex fire, in animal studies, steroids do far worse (3).
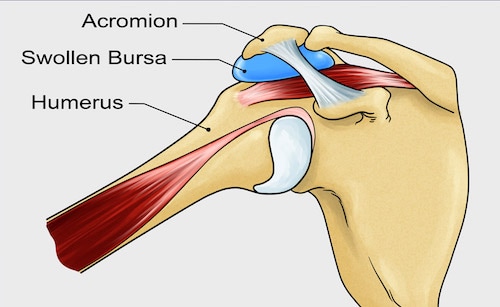
The problem? The above study showed that repeated steroid shots in this bursa really messed up the shoulder. The rotator cuff tendons reacted by getting weaker, which is not a good thing in a tendon prone to tears. In addition, the bone quality in the area went south as did the area where the tendon attached to the bone. A larger study looking at all of the basic science data concluded the same thing (4). Basically, these animal studies suggest that injecting steroids into shoulders is yet another physician caused disaster.
However, does the concept that steroids harm rotator cuff tendons extend from animals into the real world? Yep. A recent study looked at 8 papers on the subject that used real patients (5). This investigation found that corticosteroid injections in the shoulder were associated with an increased risk of revision surgery after rotator cuff repair. Basically, that the steroids were weakening the tendon so that the tendon repair surgery failed more often.
Despite this data, I continue to see patients with rotator cuff tears who get their shoulders injected with steroids. Again, this stuff is like Windex for physicians. In addition, based on the data showing that these injections hurt patients and the fact that physicians can’t seem to help themselves by continuing to routinely inject this junk, this is an addiction and nasty fatal attraction.
Can Steroids be Used Smartly Instead of Stupidly?
If you look at the research on how the body uses steroids, there’s an obvious reason why steroid shots are such a disaster. That difference is dose. Let’s dig in.
While we doctors abbreviate milligram with an “mg”, there’s another dose where we substitute the “m” with an “n”. That’s “ng”, which means nanogram. What’s the difference? A nanogram is about a million times less than a milligram.
The body uses steroids in the ng dose range. Drug manufacturers make corticosteroid drugs in the mg dose range. In our clinical experience, when you reduce the dose from mg to ng, you still get anti-inflammatory effects, but there are no crazy side effects because this is the same dose the body is used to seeing.
The upshot? It’s time we physicians end our dangerous addiction to high-dose steroid shots. The “Windex” of sports medicine needs to be retired for use in patients with orthopedic problems or pain.
______________________________
References:
(1) Benedek TG. History of the development of corticosteroid therapy. Clin Exp Rheumatol. 2011 Sep-Oct;29(5 Suppl 68):S-5-12. Epub 2011 Oct 21. PMID: 22018177.
(2) Coombes BK, et al “Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials” Lancet 2010; DOI: 10.1016/S0140-6736(10)61160-9.
(3) Maman E, Yehuda C, Pritsch T, Morag G, Brosh T, Sharfman Z, Dolkart O. Detrimental Effect of Repeated and Single Subacromial Corticosteroid Injections on the Intact and Injured Rotator Cuff: A Biomechanical and Imaging Study in Rats. Am J Sports Med. 2016 Jan;44(1):177-82. doi: 10.1177/0363546515591266. Epub 2015 Jul 27. PMID: 26216105.
(4) Puzzitiello RN, Patel BH, Forlenza EM, Nwachukwu BU, Allen AA, Forsythe B, Salzler MJ. Adverse Impact of Corticosteroids on Rotator Cuff Tendon Health and Repair: A Systematic Review of Basic Science Studies. Arthrosc Sports Med Rehabil. 2020 Apr 8;2(2):e161-e169. doi: 10.1016/j.asmr.2020.01.002. PMID: 32368753; PMCID: PMC7190543.
(5) Puzzitiello RN, Patel BH, Nwachukwu BU, Allen AA, Forsythe B, Salzler MJ. Adverse Impact of Corticosteroid Injection on Rotator Cuff Tendon Health and Repair: A Systematic Review. Arthroscopy. 2020 May;36(5):1468-1475. doi: 10.1016/j.arthro.2019.12.006. Epub 2019 Dec 17. PMID: 31862292.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
