Why Is Hip FAI Common in People Who Have No Hip Pain?
Logika600/Shutterstock
One of the real problems in modern medicine is our over-reliance on MRIs to make a diagnosis. This is rampant in the world of arthroscopic hip surgery where detecting FAI can result in an invasive procedure. Several studies have shown time and time again that while hip FAI is treated as an abnormality, it’s actually a fairly common finding in normal patients. Let’s dig in and review some brand new research.
What Is Hip FAI?
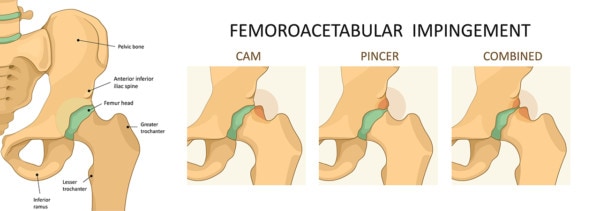
FAI stands for femoroacetabular impingement. The concept is that the hip joint is misshapen and is causing impingement. The two most common types are:
The basic idea is that the surgeon needs to remove the pincer or cam as this is resulting in damage to the hip labrum and joint. This diagnosis often leads to a labral repair or a bone removal procedure with the number of these surgeries exploding year over year (1).
What if hip FAI was a normal variant and not abnormal? If that were true, we would expect to see lots of people without hip pain who have this condition. So are there people out there who have no hip pain and who have FAI on imaging?
The Past Studies on Hip FAI in People with No Hip Pain
Let’s review some research performed on people who have no hip pain, but underwent hip x-rays or MRIs:
- A Norwegian study looked at 2.081 young adults without hip pain (2). They found that more than 50% had at least one measurement consistent with hip FAI. Many other common FAI signs were present in about a quarter of the participants.
- A US study again showed that about a quarter of the hips of people without hip pain had FAI (3).
The New Research
Enter the new research that looked at 1,878 asymptomatic hips. The researchers used 3 radiologists to make sure that the readings were correct and consistent. The mean age of these people was about 31 years old. They found that the prevalence of cam impingement was 30% and that pincer impingement was present in 24% of the individuals.
The Problem?
If hip FAI is common in 1/4 to 1/3 to 1/2 of all individuals who don’t have hip pain, then how reliable of a finding is it when someone has hip pain? Meaning given that all sorts of things can cause hip pain from the SI joint to the low back to tendons, etc…, how many people with hip pain who are diagnosed with FAI actually have this problem causing their hip pain? How many are getting operated on who had the FAI before the pain began and who have other non-FAI problems causing their hip pain?
Diagnostic Accuracy
Any reliable diagnostic test in medicine relies on it being positive only in patients with the disease and negative in those without. In this case, the disease is hip pain, because why would you care if an MRI looked abnormal but your hip was fully functional? You wouldn’t. If the test is positive in people who don’t have the disease, that’s a false positive. A reliable test has a false positive rate of 5% or less. This one, taking an x-ray or MRI to look for FAI has a false positive rate of 25-50%. In any other field of medicine, a test with a false positive rate that high would be ignored.
Does FAI Cause Hip Arthritis?
Do you know the story of the chicken or the egg? Which came first? That’s pretty much the state of the research of FAI and hip arthritis. Let me explain.
It’s possible that patients with FAI who aren’t symptomatic now may be at higher risk of developing hip OA (osteoarthritis). The only way to test that would be taking people with no hip pain where some had FAI on MRI and some did not and then follow them for many years to see who developed arthritis. Does this prospective research exist showing that asymptomatic people with hip FAI go onto develop hip OA at a greater rate than those without hip OA? Not really.
One oft pointed to study performed by the Dutch started with early symptomatic hip arthritis patients and followed them forward (5). The problem? If FAI was being caused by hip arthritis and not the other way around, this study wouldn’t have the ability to sort that out. So this study can’t be used as proof that FAI causes hip OA.
In conclusion, I was unable to find any prospective study capable of proving that FAI causes hip OA by following asymptomatic people forward. Hence, there is no hard evidence that FAI is an abnormality that causes hip OA. It may however be caused by hip OA as the natural course of the disease. Meaning that more patients that develop hip arthritis for whatever reason may also develop what looks like FAI as their disease progresses.
An Example of a Hip FAI Surgery Gone Bad
Last week I saw a 40-year-old woman in the office who was diagnosed with a cam impingement. She underwent two surgeries on that hip. They shaved off part of the femur and at first, repaired and then had to replace part of her labrum (the lip around the socket). The problem? She’s now in more pain than ever and they now want to perform a third surgery to completely replace the whole labrum.
When looking at her MRI I was shocked:
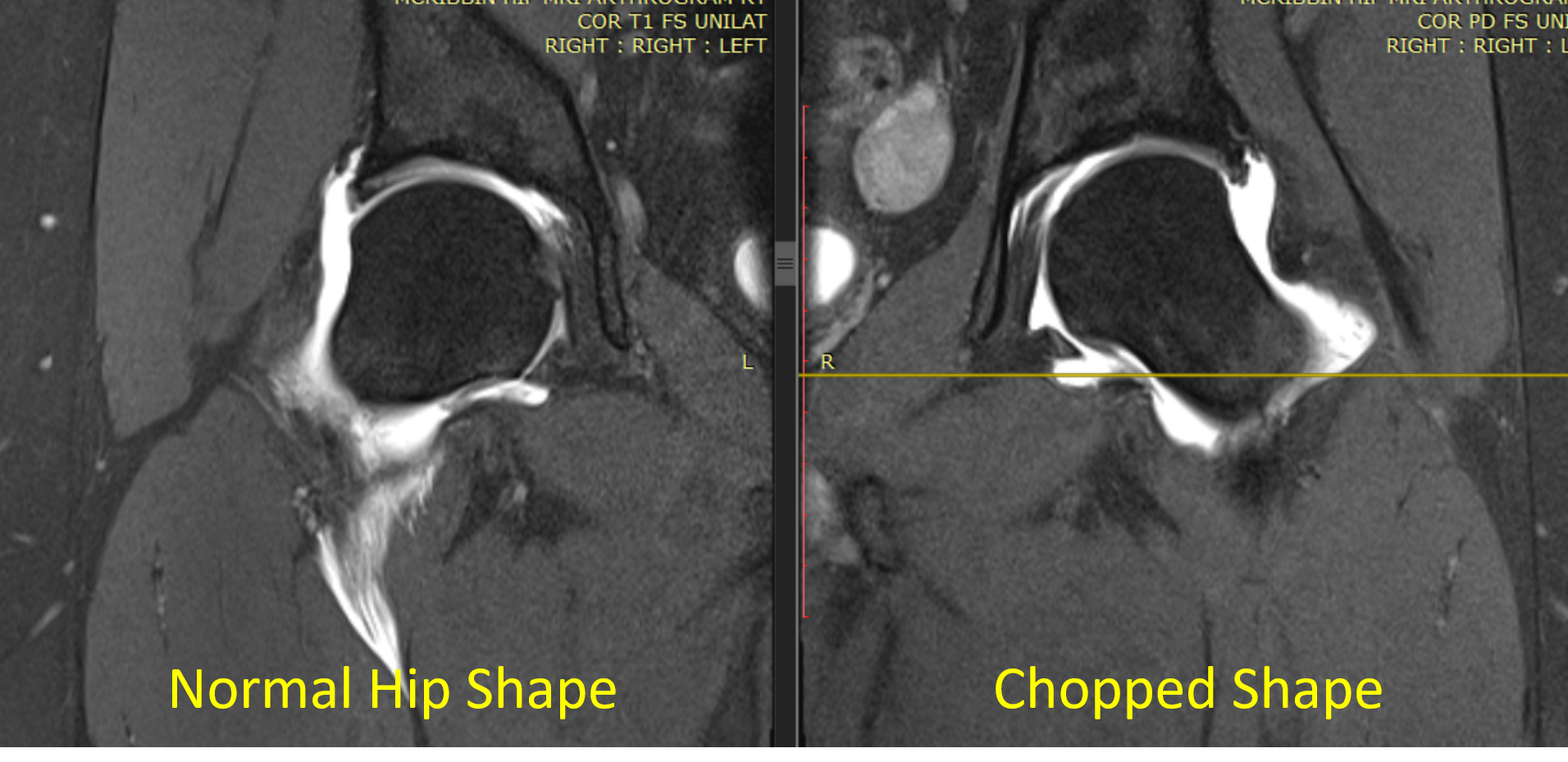
The hip femur bone on the left is the normal ice cream cone shape (spherical like a scoop of ice cream). The one on the right that has been operated on twice is now an abnormal chopped shape. Meaning too much of the outside part of the femur has been removed leaving it too small for its socket.
How Can You Avoid Being this Patient?
First, insist on a diagnostic numbing injection into the joint to confirm that your hip pain is coming from your hip joint. If it is, your pain will go away. If it doesn’t, then you could really have:
- SI joint pain referring to the hip
- A low back pinched nerve that goes to the hip
- Irritated or jacked up tendons around the hip
In addition, as shown above, we still don’t know if hip FAI causes arthritis. Hence, because lots of people are walking around out there with no hip pain and FAI on an x-ray or MRI, we need to be very cautious about operating on anyone who has FAI and hip pain. Hence, try the newer non-surgical orthobiologic options like PRP or bone marrow stem cell therapy BEFORE considering invasive surgery.
The upshot? Hip FAI is present in an awful lot of normal people with no hip pain. As a result, we need to be very careful about who we operate on and why.
_____________________________________
References:
(1) Westermann RW, Day MA, Duchman KR, Glass NA, Lynch TS, Rosneck JT. Trends in Hip Arthroscopic Labral Repair: An American Board of Orthopaedic Surgery Database Study. Arthroscopy. 2019 May;35(5):1413-1419. doi: 10.1016/j.arthro.2018.11.016. Epub 2019 Apr 9. PMID: 30979629.
(2) Laborie LB, Lehmann TG, Engesæter IØ, Eastwood DM, Engesæter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011 Aug;260(2):494-502. doi: 10.1148/radiol.11102354. Epub 2011 May 25. PMID: 21613440.
(3) Jung KA, Restrepo C, Hellman M, AbdelSalam H, Morrison W, Parvizi J. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011 Oct;93(10):1303-7. doi: 10.1302/0301-620X.93B10.26433. Erratum in: J Bone Joint Surg Br. 2011 Dec;93(12):1679. PMID: 21969426.
(4) Morales-Avalos R, Tapia-Náñez A, Simental-Mendía M, et al. Prevalence of Morphological Variations Associated With Femoroacetabular Impingement According to Age and Sex: A Study of 1878 Asymptomatic Hips in Nonprofessional Athletes. Orthopaedic Journal of Sports Medicine. February 2021. doi:10.1177/2325967120977892
(5) Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013 Jun;72(6):918-23. doi: 10.1136/annrheumdis-2012-201643. Epub 2012 Jun 23. PMID: 22730371.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
