Why Tight Pecs and Shoulder Pain Could Be a Canary in the Coalmine of the Neck

Credit: George McCaa, U.S. Bureau of Mines
Way back when, miners would take small birds into the mines, as they were sensitive to changes in oxygen and gas levels that could threaten these workers’ lives. Hence, the phrase, “canary in the coalmine” was born. This past month, with all of the graduations and events I had to attend, my left shoulder and pec showed me just how much we should be paying attention to these issues as an indicator of a neck problem. Let me explain.
I Love and Hate Getting Old
If you read this blog, you know that I both love and hate getting old. I love it because I get to experience firsthand all of these problems my patients have always talked about. There’s just no substitute for example, for experiencing what it feels like to have swollen facet joints in your back when the weather fronts move in. Nobody can teach that if you’ve never experienced it. The same is true with old age shoulder problems.
I also hate getting old for all of the same reasons you do. Frankly, if I didn’t have interventional orthobiologics to keep me going, at this point I’d likely be out of commission.
The Pec Major Muscle is Neurologically Unique
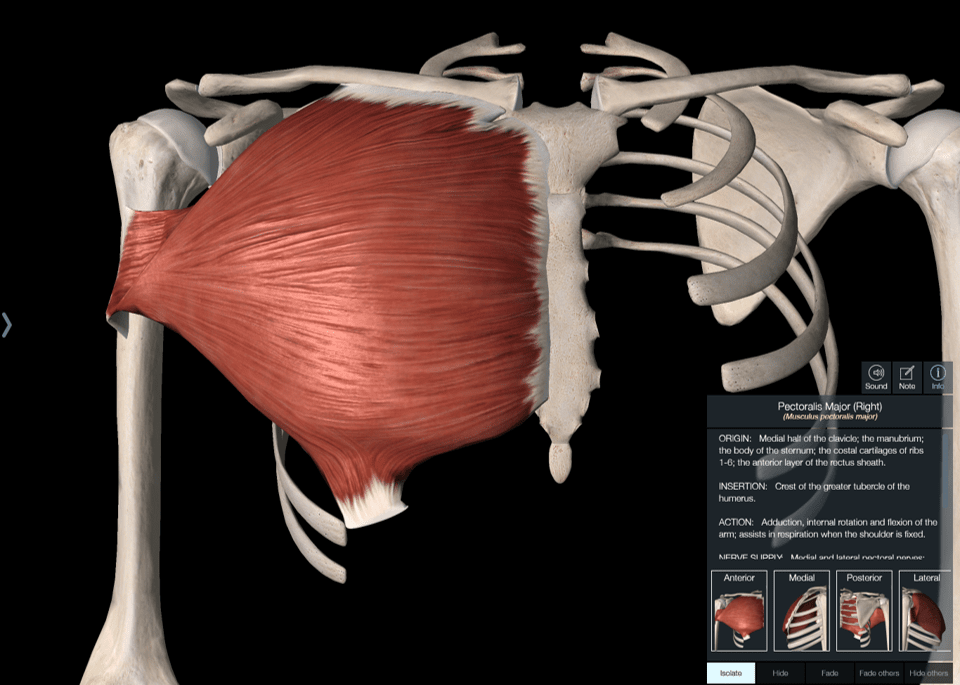
Muscles are innervated by nerves, which is how they get commands to contract and relax. Most muscles are innervated by three or fewer spinal nerves. This means that two to three specific spinal nerves coming from each level of the neck or back supply that muscle. For example, your calf muscle (gastrocnemius) is supplied by the S1 and S2 spinal nerves. Your butt muscle (gluteus maximus) is innervated by the L5, S1, and S2 nerves. However, the pec muscle in the front of your chest is innervated by 5 spinal nerves! In fact, all of those nerves happen to be in the region of the neck most impacted by degenerative disc disease. Those are the C5, C6, C7, C8, and T1 nerves.
The Canary in the Coalmine of the Neck
While I’ve known about this unique innervation of the pec for a very long time, there’s nothing like real-world experience with getting old to make you understand something at a gut level. I have a neck that looks like it needed surgery 5 years ago when I had severe neck and back of shoulder pain. In fact, a family friend (who is now not doing well) had a neck fusion at that same time for a less impressive MRI. I, on the other hand, had my Colorado colleagues perform our cervical platelet-based DDD procedure. So I never had surgery. Instead, every few years I get a touch-up neck platelet injection and otherwise still lift heavy weights and do everything else I want.
However, this past month has been a bit rough on my old neck. It began with an out-of-state wedding, then college and high-school graduations with many different events each. Between planes and lots of bleachers and parties that went late and mornings that were far too early, my neck began getting a bit sore. However, what really hurt was my left shoulder. While I knew this could be coming from my neck, this pain seem to center around my left AC joint, which I had injured in a motorcycle accident when I was in my 20s. That joint felt very unstable and painful with any kind of lifting.
A few weeks ago, I was driving home and my left shoulder was aching, so I instinctively went to my pec to massage out some trigger points. I wondered at the time, whether the spinal nerves in my neck were messing with my pec muscle and that was causing bad shoulder biomechanics. Meaning, at the time, I couldn’t lift my shoulder without getting cracking and popping in my left shoulder which would eventually lead to aching pain. That pain was getting unbearable after lifting weights or even carrying anything on that side. After my self-massage of the pec major trigger points, I was amazed that I could immediately lift my shoulder without any popping and cracking. In addition, the severe shoulder aching disappeared as I hit these spots with more and more vigor. So what happened?
What Is a Muscle Trigger Point?
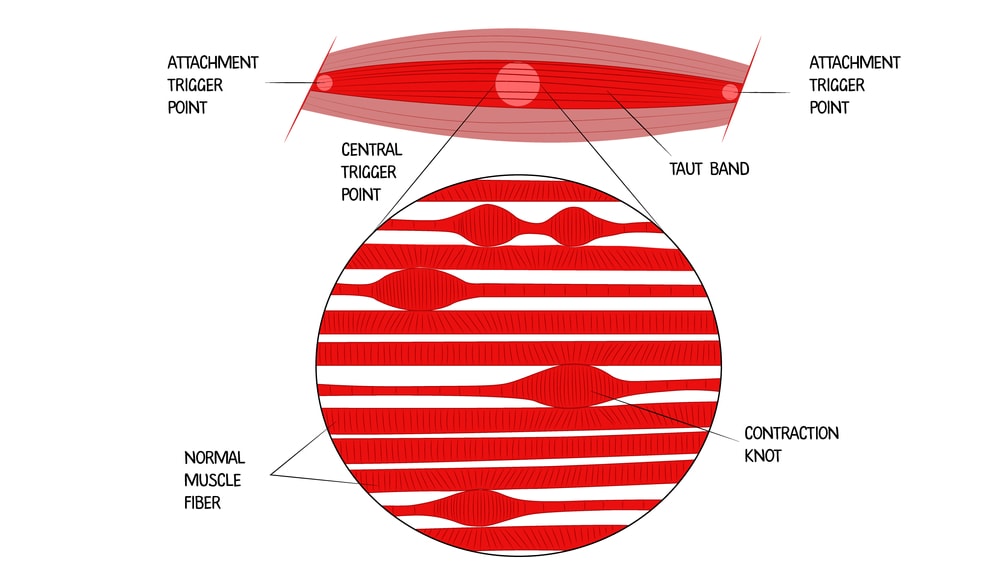
Credit: Shutterstock
You probably know that you have knots that can crop up in your muscles. These taut bands are called “trigger points”. They aren’t random, but often due to problems in the nerve innervating that muscle. They can cause havoc because these parts of the muscle don’t contract and relax normally. Hence, they make the whole muscle contract unevenly.
The pec major muscle is an internal rotator of the shoulder joint that also can bring the humerus (arm bone) closer to the mid-line. When you raise your shoulder, the pec muscle must let go with millisecond accuracy. If it has trigger points, it can’t do that, so it impacts how the shoulder moves, placing too much downward pressure on the joint. That beats up the main shoulder and AC joint, which leads to deep aching shoulder pain.
Is Your Shoulder Pain Related to Your Neck?
While my old man’s neck and shoulder might be interesting, how does this relate to your shoulder and neck? First, is your pec major muscle tight and destroying the biomechanics of your shoulder? One way to easily test this is to place firm pressure for 10-20 seconds on the knots you find in that pec major muscle. This may take a few minutes to find all of the spots, but if that improves your shoulder range of motion and pain, you may have the same issue.
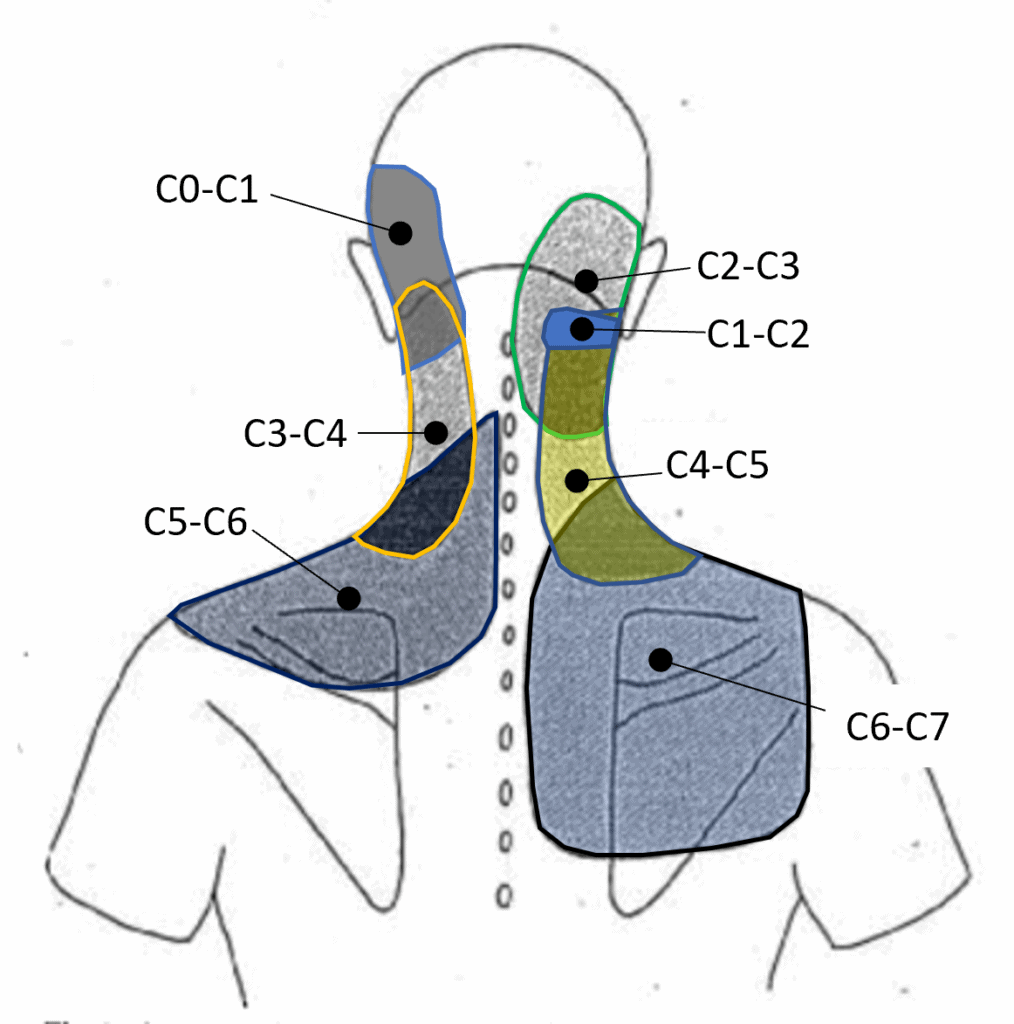
Credit: Heavily modified image taken from Dwyer et al
Second, realize that there is often a connection between shoulder pain and the neck that can go beyond this pec problem. That’s because irritated neck nerves can refer pain to the shoulder. These irritated nerves can also impact the function of other muscles like those in the rotator cuff. Finally, lower neck problems like arthritic facet joints at C5-C7 can refer pain to the upper trap and shoulder blade areas (see above). Hence, any patient with shoulder pain should be asked if they also have a neck issue and if so, an exam of both the shoulder and the neck should be standard.
The upshot? As I said, I love getting old and experiencing all the stuff my patients have complained about for years. My shoulder is just the latest example. Just realize the next time your shoulder hurts, think for a second if it could be coming from your neck!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
