Why We Should Be Paying More Attention to Macrophages
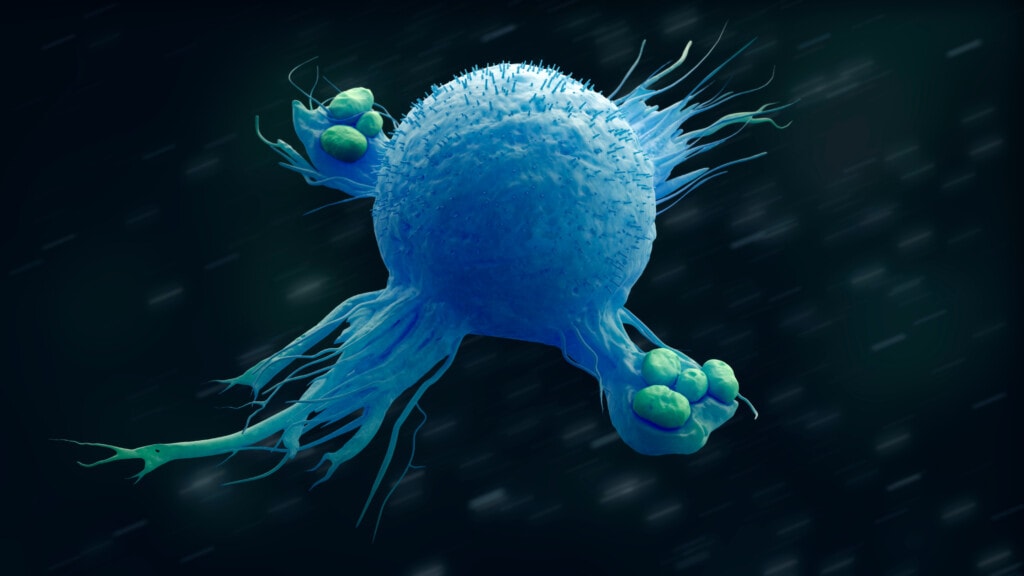
Credit: Shutterstock
Way back when in medical school, when the topic of macrophages came up, we learned that they were the garbage men of the body in that they got rid of bacteria and dead tissue. However, less known then was how these large cells assisted in tissue repair. So let’s learn about macrophages and their critical role in determining if PRP is effective in helping osteoarthritis in patients treat the ravaging effects of chronic inflammation.
Macrophages 101
The traditional definition of a macrophage is:
“A type of white blood cell that surrounds and kills microorganisms, removes dead cells, and stimulates the action of other immune system cells.” (1)
They are giant cells at 21 micrometers; compare that to the size of red blood cells at 7-8 micrometers, and you get a sense of how massive they are in this microscopic world (2). This enormous size is the reason for the first part of their name, “macro,” which derives from makrós in ancient Greek which means “large.” Above is an image of a macrophage engulfing bacteria, which is part of the old-school definition which gave them the last part of their name. They “eat” debris and foreign invaders, hence the “phage” (phageîn in ancient Greek means “to eat”).
The Many “Jobs” of Macrophages
While it’s interesting to know that macrophages have this garbage man function, what many don’t realize is that they also play a critical role in stoking and controlling inflammation and, more critically, in why the type of chronic inflammation created by 1st world diseases like metabolic syndrome can destroy joints. It’s their different states that allow them to do three different “jobs” in injury and tissue repair.
Macrophages come in three states:
- MO (inactivated)
- M1 (pro-inflammatory)
- M2 (anti-inflammatory)

Credit: Author with Some Images from Shutterstock
M0 macrophages lie dormant, waiting for something to happen. M0 macrophages convert to the M1 state when exposed to a pro-inflammatory stimulus. Hence, if there’s an acute injury, the local cytokines released to stoke the acute inflammatory “fire” will switch the M0 resting state macrophages into M1 “Pro-inflammatory Mode.” These M1 cells then excrete more pro-inflammatory cytokines amplifying the local injury response, which brings in other repair cells. They also release substances that can kill bacteria, and they eliminate injured and dead tissue. Think of them as the “demolition crew” in a remodeling project. They are like a demotion crew taking down the old damaged building and carting the debris off the construction site.
In normal acute inflammation, after a few days of demolition, things need to switch from inflammation to the repair part of the response, where new tissue is being laid down to heal the damage. This happens when the M1 macrophage detects certain cytokines in the area associated with the resolution of inflammation. In normal healthy individuals, the M1 macrophages then convert to the M2 state and are involved in collagen production and tissue repair, as well as the release of cytokines to continue to quash inflammation (anti-inflammatory). Using our construction site analogy, the demo crew now changes job descriptions to become the building crew.
Macrophages in Chronic Inflammation?
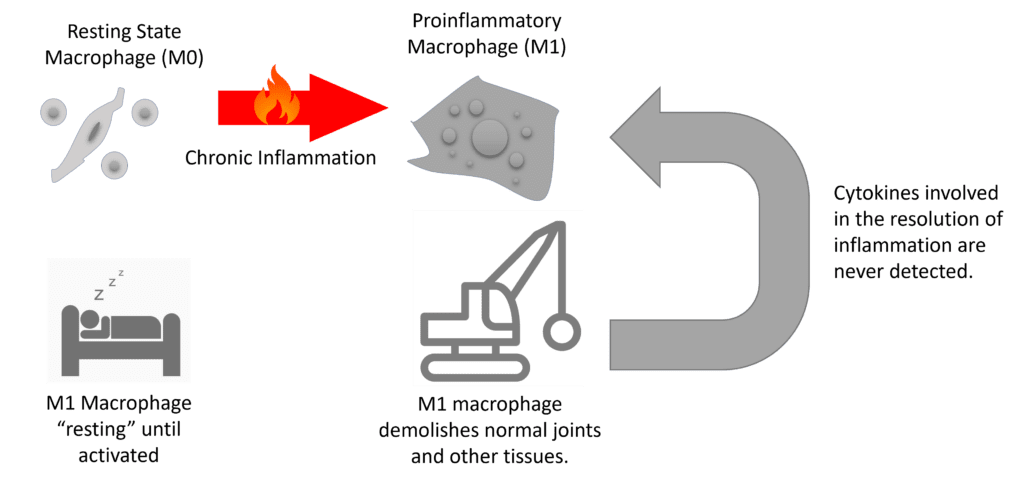
Author with Some Images from Shutterstock
What happens if the bad M1 macrophages continue to detect that there are pro-inflammatory chemicals in their area and never detect the cytokines involved in the resolution of inflammation? They stay in that “demo crew” M1 state and continue to destroy things and excrete more pro-inflammatory cytokines that wreak havoc. That’s one of the mechanisms behind joint arthritis and other maladies like heart disease in patients with chronic inflammation due to metabolic syndrome.
Given that many of our patients in the first world have this type of arthritis caused by chronic inflammation, for orthobiologic treatments to be effective, they would need to help shift these M1 demolition macrophages to the pro-repair M2 type. Let’s look at some research on how platelet-rich plasma impacts that dynamic.
Can PRP Force Bad M1 Macrophages into the M2 Good Guys?
Here’s a sample of the existing research on PRP and macrophage polarization (moving a macrophage from one state to another):
- Exosomes derived from platelet-rich plasma reduced the formation of the pro-inflammatory demolition M1 macrophages in an animal model of spine DDD. (3)
- PRP in a hydrogel was able to recruit the pro-repair M2 macrophages or turn inactivated (resting state M0) macrophages into the anti-inflammatory M2 type. (4)
- Macrophages that were induced into the pro-inflammatory M1 state and then treated with platelet lysate were converted to pro-repair M2 macrophages that began excreting anti-inflammatory cytokines and stimulated fibroblast cells to make collagen (indicating the stimulus of repair). (5)
- Adding PRP to macrophage cultures again reduced the M1 pro-inflammatory type and increased the anti-inflammatory, pro-repair M2 type. (6)
The upshot? It’s time to begin paying attention to what macrophages do and how important they are in tissue repair. Hopefully, the idea that macrophages are mere cellular garbagemen will be “trashed”!
______________________________________________________________
References:
(1) NIH. National Cancer Institute. Macrophage. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/macrophage Accessed 1/25/23
(2) Gordon S. The macrophage: past, present and future. Eur J Immunol. 2007 Nov;37 Suppl 1:S9-17. doi: 10.1002/eji.200737638. PMID: 17972350.
(3) Qian J, Wang X, Su G, Shu X, Huang Z, Jiang H, Zhu Q. Platelet-rich plasma-derived exosomes attenuate intervertebral disc degeneration by promoting NLRP3 autophagic degradation in macrophages. Int Immunopharmacol. 2022 Sep;110:108962. doi: 10.1016/j.intimp.2022.108962. Epub 2022 Jun 24. PMID: 35753124.
(4) Pan X, Yuan S, Xun X, Fan Z, Xue X, Zhang C, Wang J, Deng J. Long-Term Recruitment of Endogenous M2 Macrophages by Platelet Lysate-Rich Plasma Macroporous Hydrogel Scaffold for Articular Cartilage Defect Repair. Adv Healthc Mater. 2022 Mar;11(6):e2101661. doi: 10.1002/adhm.202101661. Epub 2022 Jan 7. PMID: 34969180.
(5) Scopelliti F, Caterina C, Valentina D, Gianfranco C, Concetta M, Andrea C. Platelet lysate converts M (IFNγ+LPS) macrophages in CD206+ TGF-β+ arginase+ M2-like macrophages that affect fibroblast activity and T lymphocyte migration. J Tissue Eng Regen Med. 2021 Sep;15(9):788-797. doi: 10.1002/term.3229. Epub 2021 Jul 31. PMID: 34311512.
(6) Uchiyama R, Toyoda E, Maehara M, Wasai S, Omura H, Watanabe M, Sato M. Effect of Platelet-Rich Plasma on M1/M2 Macrophage Polarization. Int J Mol Sci. 2021 Feb 26;22(5):2336. doi: 10.3390/ijms22052336. PMID: 33652994; PMCID: PMC7956636.
(7) Berger DR, Centeno CJ, Steinmetz NJ. Platelet lysates from aged donors promote human tenocyte proliferation and migration in a concentration-dependent manner. Bone Joint Res. 2019 Feb 2;8(1):32-40. doi: 10.1302/2046-3758.81.BJR-2018-0164.R1. PMID: 30800297; PMCID: PMC6359887.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
