Will Exercise Make My Arthritis Worse: MRI May Help Decide
I often see active patients in clinic who want to know if exercise will make their arthritis advance. They’ve seen friends be hobbled by knee replacement who drop out of high-level physical activity, and they don’t want that fate. Several studies over the last few years do support the idea that it may be possible to use certain MRI findings to answer the question, “Will exercise make my arthritis worse?”
What Is Knee Arthritis and What Does MRI Show?
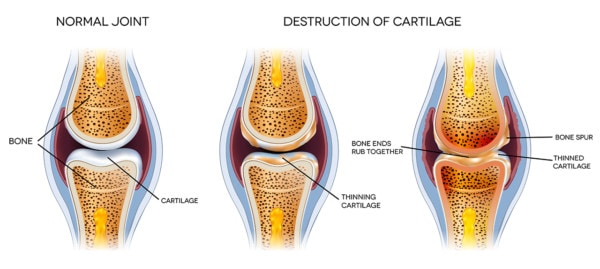
The progression of Knee arthritis. Tefi/Shutterstock
Knee arthritis is diagnosed when the knee loses cartilage, develops bone spurs, and develops a toxic environment in the joint, and all of that is associated with pain and lost function. An MRI image can tell us the status of the cartilage and bone, but it can also see more. One finding that’s very interesting is called a “bone marrow lesion,” or BML. This is swelling in the bone due to microfractures. More advanced forms of MRI, like T2 mapping, use a color-coded map of the amount of water in the cartilage to provide more detail of its health.
Will Exercise Make My Arthritis Worse?
This has been a back and forth question for years, with some studies showing that high-impact exercise, like running, can make arthritis worse and some going the other way, showing that runners have less arthritis. The reason these studies go in both directions may have to do with the status of the cartilage in the subjects when the study begins. Meaning that patients with no pain or functional problems but who have unhealthy cartilage or bone may get worse with exercise while others with no such issues may be protected by exercise. Hence, if your study includes more subjects with no problems but slightly unhealthy cartilage, it shows that exercise causes arthritis versus another study that begins with more patients with good cartilage that will show that exercise protects against arthritis.
New MRI Studies Seek to Answer the Question
The new research studies actually took MRIs of the knees of patients before the study began to get an idea of cartilage health when there were no complaints of pain or lost function. One study looked at the presence or absence of BMLs, theorizing that if one was present, the health of the bone and cartilage was poor. In this study, patients with BMLs had progressive cartilage loss with exercise while patients with no BMLs had no cartilage loss. In another study, sophisticated T2 mapping of the cartilage health was performed, showing that patients with less healthy cartilage went on to lose it with exercise versus those with healthy cartilage, who kept it with exercise.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
