Your Ligaments Respond to Force!
All of your ligaments are alive. What I mean by that is that they respond to forces because they have living cells. Let’s dig in.
Ligaments Are the Duct Tape that Hold Your Bones Together
The ligaments hold bones together like pieces of duct tape. They stabilize your joints as they get toward their maximum range of motion. Ligaments, when damaged, are often replaced, which views them like inanimate pieces of tape. However, how would ligament replacement surgery be impacted if ligaments were alive and constantly adapting to force?
Ligament Volume and Activity
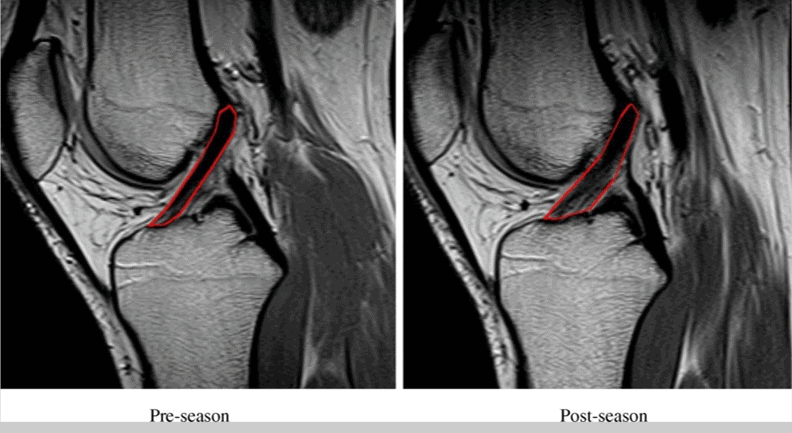
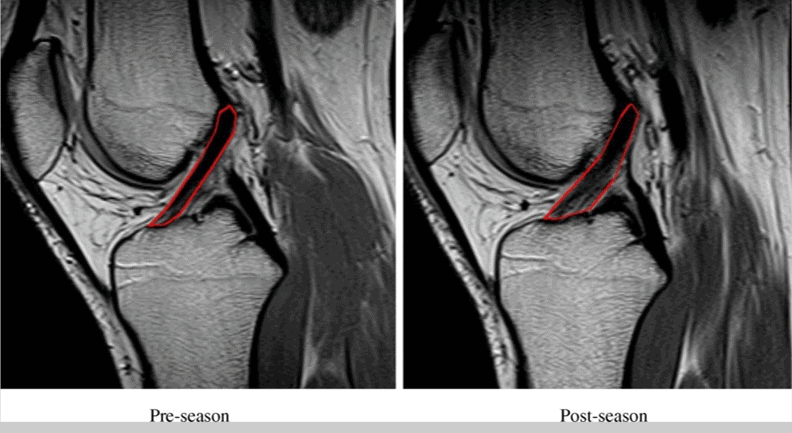
In this new study, 14 Division-I college soccer players were recruited. A high-resolution MRI was taken of their knee ACL ligaments at the beginning of the season. Contours of the ACL were outlined in sagittal T-2 weighted MR images and volumes were calculated using Medical Image Processing, Analysis, and Visualization software. The initial goal of the study was to detect occult ACL injury during the season, so a second MRI was taken at the end of the study. The results? The ACLs got significantly bigger at the end of the season! See above for the images from the study.
Why Is This Happening?
The healthy ACL is filled with cells that help repair any damage that happens with day-to-day living. Now we know that these cells respond to increased demand by increasing the size of the ligament. This fits with what I’ve been saying for years and what medical science has known for a century, that every part of your body is alive and reacts to force. It also fits with the results we have seen on MRI when we inject the patient’s own cells into the ligament.
What Are the Implications for Ligament Surgery?
When ligaments are damaged, a traditional old-school way to repair them is to remove the ligament and replace it with either:
- a tendon from the patient
- an artificial ligament
- a ligament from a cadaver
The problem is that only one of the above will have live cells that will respond to demand like the original ligament. A tendon from the patient is the only one that has a chance to react normally to force. However, that repair will never be like the original equipment in that the knee will now lack position sense, have more rotational instability, and have an artificial ligament that is steeper than the original.
Is There Another Way?
What if we could save the damaged ligament and get it to repair itself? That’s what we do at Regenexx. For selected patients, we use highly precise image-guided injections of the patient’s own bone marrow concentrate into the damaged ligament. That way, you get to keep your original equipment. See my video below on the ACL procedure:
The upshot? This new study proves a point. It shows that our ligaments respond to what we do and constantly repair themselves. That means that keeping your original equipment that responds to the demands you place on your body is more important than ever!
______________________________
References;
(1) Myrick KM, Voss A, Feinn RS, Martin T, Mele BM, Garbalosa JC. Effects of season long participation on ACL volume in female intercollegiate soccer athletes. J Exp Orthop. 2019 Mar 28;6(1):12. doi: 10.1186/s40634-019-0182-8. PMID: 30923976; PMCID: PMC6438997.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
