
Medically Reviewed By:

A shoulder labral tear occurs when the labrum, a ring of specialized cartilage that cushions and stabilizes the shoulder joint, becomes torn or damaged. This injury may result from trauma, repetitive overhead motion, or age-related degeneration. Common symptoms include shoulder discomfort, instability, and restricted motion.
Initial treatment often begins with medications that help reduce symptoms, but these may not address underlying issues such as rotator cuff involvement or degenerative joint conditions. In more severe cases, surgery may be recommended to stabilize the joint, though this approach carries risks such as infection, prolonged recovery, and inconsistent outcomes.
At Active Life Physical Medicine & Pain Center in Phoenix, AZ, physicians in the licensed Regenexx network offer procedures using Regenexx injectates as part of a non-surgical strategy for managing labral-related shoulder pain. These procedures utilize interventional orthobiologics to support the body’s natural repair response and may help reduce the need for invasive surgery or long-term prescription medication use.
Shoulder Labrum: Structure And Function
The shoulder connects three primary bones:
- Humerus – the upper arm bone
- Scapula – the shoulder blade
- Clavicle – the collarbone
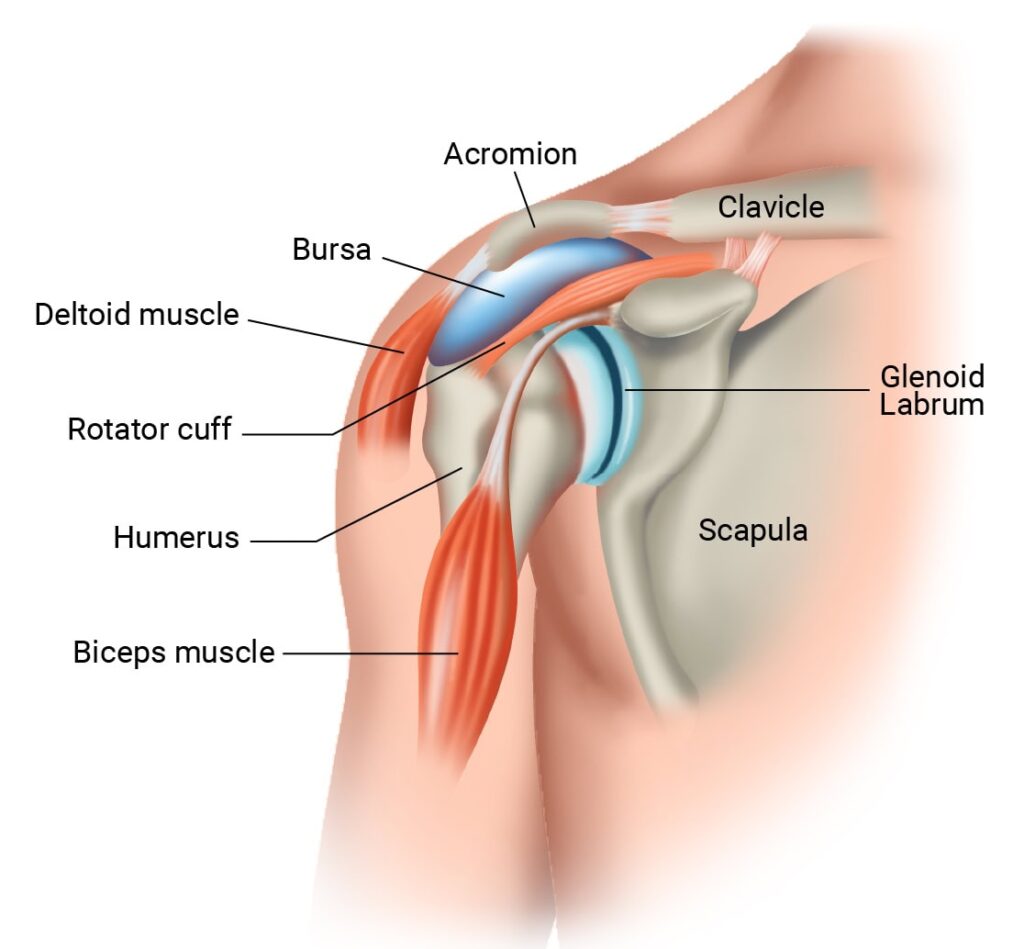
The glenohumeral joint (shoulder’s ball-and-socket) allows wide-ranging motion but relies on soft tissue for stability due to its shallow socket.
The labrum is a thick ring of cartilage around the socket that deepens the joint and stabilizes the humeral head. It functions like a bumper to keep the shoulder aligned during motion.
What Is a Labral Tear in the Shoulder?
Labral tears are injuries to the cartilage that lines the shoulder socket. They occur when repeated stress or trauma causes the collagen fibers in the labrum to tear or separate. These injuries are common with age and among individuals involved in high-demand physical activity, such as sports.
Labral tears may be acute or traumatic. They can result from a sudden force or shear stress that moves parts of the cartilage in opposite directions, causing tearing or fraying. A 2019 study reported that one-quarter of asymptomatic ice hockey players showed MRI findings consistent with labral tears.
In some cases, labral damage may follow another injury to the shoulder. Common causes include:
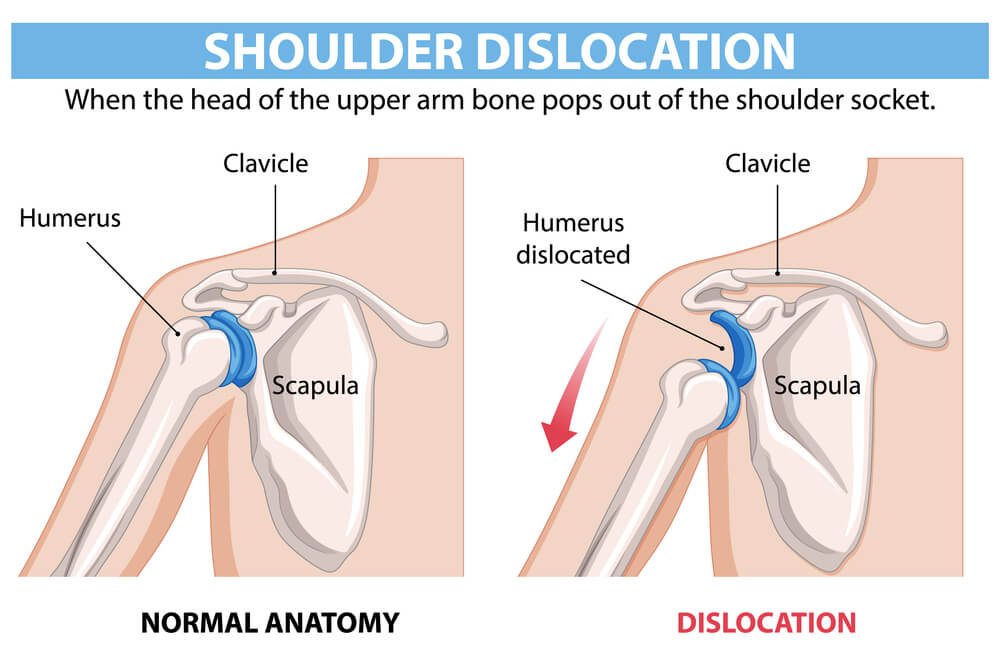
- Dislocations: When the shoulder bone is pushed out of its normal position in the joint.
- Subluxations: A partial dislocation, where bones are misaligned but not fully displaced.
When the shoulder is forced out of place, it can place stress on the labrum. This pulling force may result in a tear.
Types of Labral Tears in the Shoulder
Labral tears are identified by their location, extent, and underlying cause:
- Anterior labral tear (Bankart lesion): This tear affects the front of the labrum and is often caused by dislocation or repeated overhead movement.
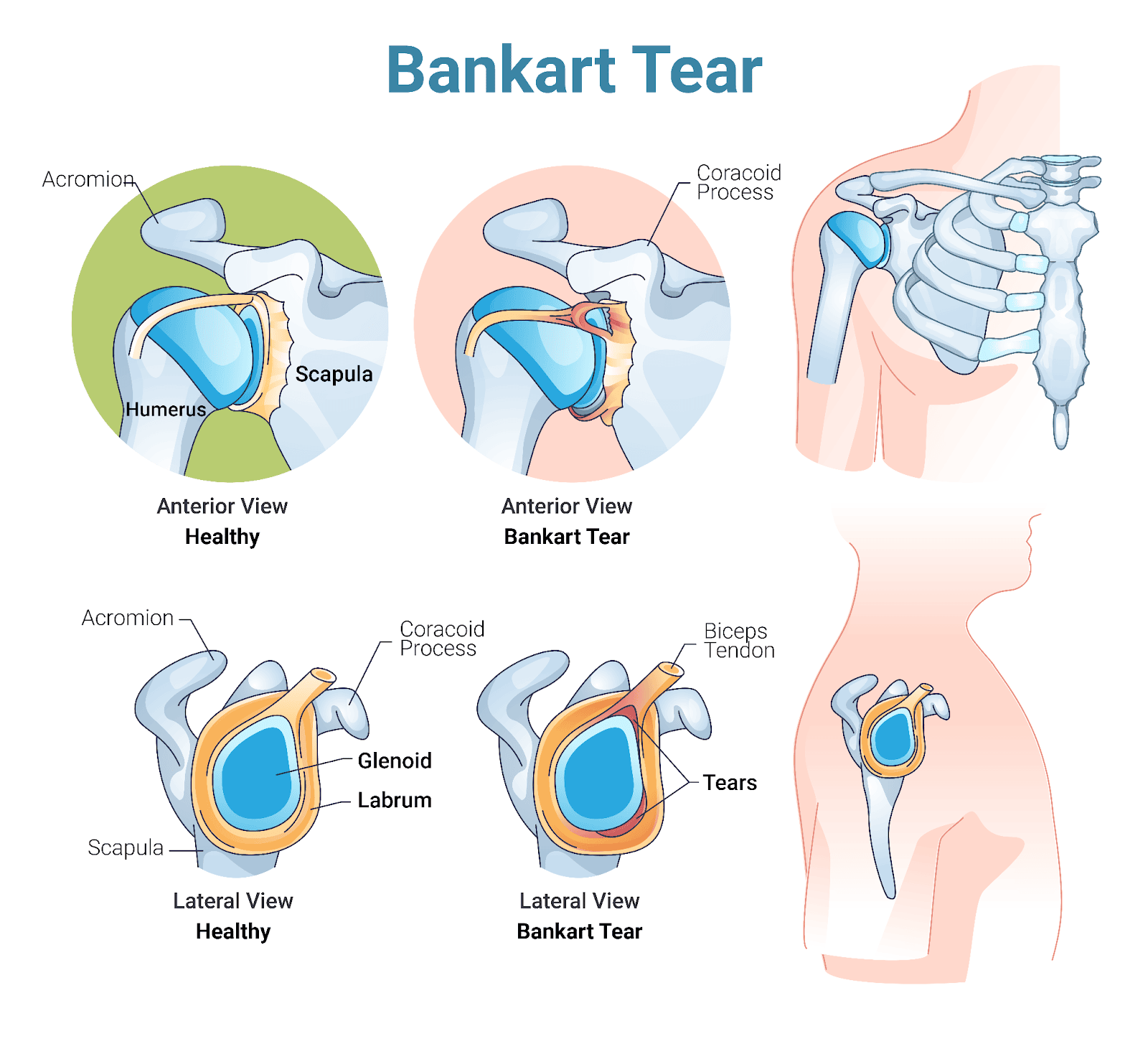
- Posterior labral tear (Reverse Bankart lesion): This tear occurs at the back of the labrum, often due to repeated compression or twisting, such as during weightlifting or rowing.
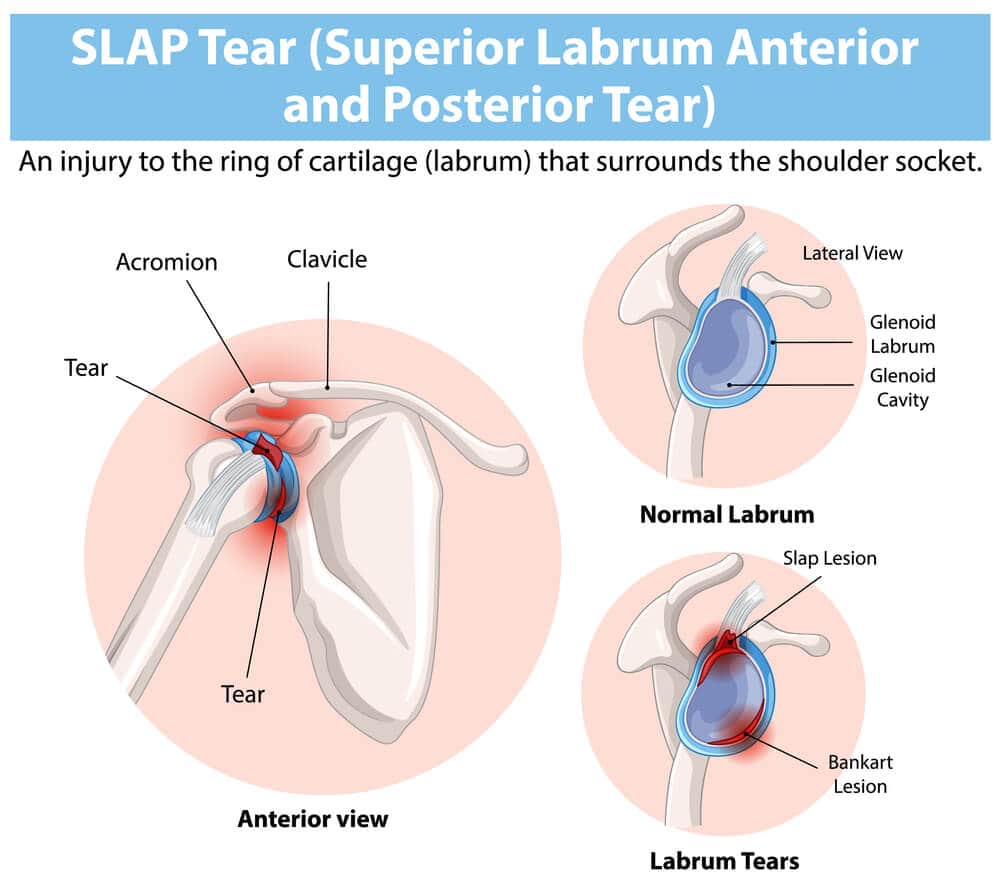
- Superior labrum, anterior to posterior tear (SLAP tear): This tear occurs at the top of the labrum where the biceps tendon attaches. It may lead to pain and instability by weakening this attachment.
- Degenerative labral tear: Typically related to aging or wear over time, this tear may appear alongside osteoarthritis and progress gradually.
Labral Tears Symptoms
Labral tears may not always cause noticeable symptoms. One study found that up to 70% of asymptomatic individuals showed labral changes on MRI.
However, the following symptoms are commonly reported:
Pain and Swelling
Discomfort is often felt deep in the shoulder and may be accompanied by inflammation and fluid accumulation.
Popping, Locking, or Grinding in the Joint
A tear may cause a popping sensation at the time of injury. Ongoing movement may then produce locking or grinding.
The grinding sound, known as crepitus, occurs when the uneven edges of the torn labrum interfere with joint motion, sometimes causing audible noise or discomfort.
Loss of Range of Motion
Restricted movement may result from swelling or mechanical obstruction caused by the tear.
Shoulder Dislocation
Tears may increase the risk of dislocation by reducing joint stability. Once dislocated, the shoulder may become more vulnerable to further dislocations, which can cause repeated injury to the labrum.
Recurrent dislocations may worsen the damage over time. When labral damage contributes to frequent dislocations, a physician may consider surgery. This option carries risks, such as infection, ongoing instability, and injury to nearby joint structures.
Recovery from surgery may require six to twelve months.
Instability and Weakness
A torn labrum may cause a sensation of the shoulder “giving way,” especially during overhead or throwing motions. This happens when the labrum is unable to maintain proper alignment in the joint.
Difficulty Sleeping on the Affected Side
Shoulder pain may interfere with sleep, particularly when lying on the affected side. Accidental pressure on an inflamed joint can increase swelling, leading to discomfort and disrupted sleep.
- Throbbing Pain in the Arm: A pulsating sensation that extends from the shoulder to the wrist may worsen during repetitive use. Read More About Throbbing Pain in the Arm.
Investigating the Causes and Risk Factors
Shoulder labral tears fall into two groups:
- Acute tears: These may occur from sudden trauma to the arm, such as falling on an outstretched hand.
- Degenerative tears: These result from gradual cartilage wear, often related to age or repeated shoulder use.
Causes and risk factors include:
- Frequent overhead movements: Activities like throwing or lifting may create small injuries known as microtrauma. Repeated microtrauma can eventually lead to tearing.
- Poor posture: Forward head position or slouching may place strain on the shoulder and increase the risk of labral injury.
- Degenerative changes: Age-related breakdown of joint cartilage may lead to tears, even in the absence of a specific injury.
- Glenoid bone irregularities: Structural issues with the shoulder socket may increase the labrum’s susceptibility to damage.
- Connective tissue disorders: Conditions such as Ehlers-Danlos syndrome may increase joint looseness, causing additional stress and friction that may result in labral degeneration.
- Scapular dyskinesis: Altered movement patterns in the shoulder blade may lead to faster wear of the labral tissue.
- Prolonged crutch use: Improper or extended use of crutches may strain the shoulder joint and increase the chance of labral damage over time.
- Previous shoulder surgeries: Scar tissue and changes in joint mechanics following surgery may contribute to future labral tears.
Sports with high shoulder demand: Activities such as swimming, gymnastics, or occupations requiring repetitive shoulder use may elevate the risk of labral injuries through ongoing joint stress.
Diagnosing a Labral Tear in the Shoulder
Evaluation at Active Life Physical Medicine & Pain Center may include:
- Symptom and medical history review: This includes prior dislocations, genetic conditions, or past shoulder surgeries.
- Physical examination: Specific movements may be performed to identify pain patterns or joint instability.
- Magnetic resonance imaging (MRI) or ultrasound: These techniques provide visualization of soft tissues to assess labral integrity.
- X-rays: Used to exclude bone abnormalities or fractures that may mimic labral symptoms.
Conventional Treatment Options
Conventional treatments focus on reducing symptoms and improving shoulder function. These include both non-surgical and surgical approaches.
Non-Surgical Treatment Options
Non-surgical care is often the first step in managing shoulder labral tears. These methods are designed to address symptoms and support recovery without requiring invasive procedures:
- Conservative management: Modifying activity and allowing rest may help reduce strain and support healing.
- Physical therapy: A targeted program designed by a physical therapist may help improve flexibility and strengthen shoulder support muscles.
Surgical Interventions
Surgery may be considered when labral tears cause significant disability or when conservative treatments have not improved symptoms. Surgical procedures aim to restore joint function and stability. Options include:
- Arthroscopic repair: This minimally invasive approach uses a small camera and surgical tools inserted through small incisions to repair the labrum.
- Labrum repair surgery: A more extensive procedure in which the torn labrum is reattached to the bone using small anchors.
Surgical procedures carry potential risks, such as infection or extended recovery times. A study also highlights possible complications:
- Anchor failure: The small devices used to reattach tissue may fail due to poor placement or wear.
- Chondrolysis: A rare complication that causes rapid cartilage breakdown and joint space narrowing.
How Successful Is Shoulder Labrum Repair Surgery?
Labral tear repair may involve reattaching the biceps tendon to a different part of the shoulder to improve stability. Although this procedure may be effective for some individuals, it typically includes a period of rehabilitation with physical therapy and carries certain risks.
In some cases, surgery may not fully address the underlying causes of instability, increasing the chance of recurrence. Discussing all available treatment options with a physician is essential to determine the most appropriate plan of care.
Can Recovery from Tears Be Accelerated Without Surgery?
It is a common belief that surgery leads to significant pain relief, but outcomes may vary. In some cases, surgical interventions do not meet expectations.
A 2021 study reported post-surgical complications such as subluxation, dislocation, and ongoing instability. Some patients also required revision procedures. All surgical interventions carry risks, including infection and prolonged rehabilitation.
It is important to note that not all shoulder labral tears require surgery. Many individuals can improve shoulder function without undergoing invasive procedures and the risks they present.
At Active Life Physical Medicine & Pain Center in Phoenix, AZ, procedures using Regenexx injectates offer an alternative approach. These image-guided procedures are designed to target tissue damage and support the body’s natural ability to heal.
Regenexx’s Approach to Improving Shoulder Function
The Regenexx approach utilizes orthobiologic injectates, prepared using Regenexx lab processes, to promote soft tissue repair without surgery. Treatment begins with a detailed evaluation by a physician in the licensed Regenexx network.
Personalized care plans may include one or more of the Regenexx injectates described below:
Regenexx SD Injectate
Procedures using Regenexx-SD injectate follow a patented protocol utilizing Bone Marrow Concentrate (BMC), which contains the patient’s own mesenchymal stem cells. Regenexx lab processing routinely achieves 20x cell concentration—significantly higher than typical non-Regenexx methods.
Regenexx SCP Injectate
Regenexx-SCP injectate is an enhanced form of platelet-rich plasma (PRP). Blood is collected and processed to isolate and concentrate platelets and growth factors, which are then precisely injected into the shoulder using imaging guidance. This procedure provides a higher concentration of growth factors compared to standard PRP.
Regenexx PL Injectate
Regenexx-PL injectate is a specialized derivative of PRP that delivers a faster, more concentrated release of growth factors. It is often combined with PRP or Bone Marrow Concentrate as part of a broader orthobiologic protocol.
Help Improve Shoulder Function Without Surgery
Shoulder labral tears can disrupt daily activities and overall quality of life. If conventional care has not delivered lasting relief and surgery seems premature or undesirable, Regenexx procedures may offer another path forward.
At Active Life Physical Medicine & Pain Center in Phoenix, AZ, procedures using Regenexx injectates may help improve stability and function while reducing reliance on medications or invasive treatments.
16620 North 40th Street
Phoenix, AZ 85032
Request an Appointment
Call to Schedule Schedule OnlineClinic Hours
| Sunday | Closed |
| Monday | 7:30AM–5PM |
| Tuesday | 7:30AM–5PM |
| Wednesday | 7:30AM–5PM |
| Thursday | 7:30AM–5PM |
| Friday | 7:30AM–3PM |
| Saturday | Closed |
Request an Appointment

Medically Reviewed By:
