SI Joint Fusion Surgery Side Effects: This is a Dumb Idea
The sacroliac joint (SI) has always been a controversial topic in medicine. How to effectively treat patients with chronic SI joint problems has also been a mystery to many physicians. A new take on an old and defrocked surgery called SI Joint fusion is now becoming all the rage, but should patients with SI joint pain be fooled by the slick advertising? In other words, what are SI joint fusion surgery side effects vs. benefits?
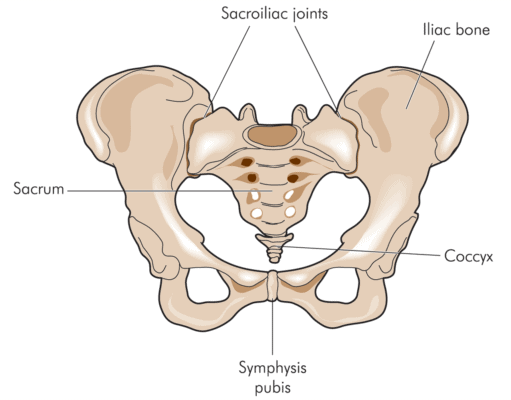
The SI joint is located where the tailbone (sacrum) meets the ilium (back of the hip). For many years (i.e. when I began treating patients in the 80s), surgeons swore on a stack of Bibles that the joint didn’t move and could cause no pain. It really wasn’t until about 2000 that most surgeons agreed that the joint acted as an important energy transfer mechanism from the legs to the spine by stretching and allowing small movements. In addition, several studies in the 90s began to show that the joint could be injected and that this could help patients with SI joint pain.
Blamb/Shutterstock
The history of SI joint surgery is filled with lots of disasters. The surgery was momentarily popular in the 90s, but it soon became out of fashion as surgeons began to observe that fusing this joint would cause other problems and pains. In fact, it’s a well established medical fact that fusing any part of the spine (bolting it together so it won’t move) means that other parts of the spine get overloaded as they compensate for the lack of motion. These other non-fused areas then begin to break down and get arthritis, causing more long-term problems. This phenomenon takes about 9-12 months to really show up, so if you want to design an SI joint fusion study to show that the surgery worked, you would only run the study for about 6 months. This is exactly the type of bait and switch research which has regrettably appeared and will prompt many patients to get this disastrous and life changing surgery.
The new study was sponsored by the company that makes the extraordinarily expensive hardware to fuse the SI joint and was published in March on 148 patients with SI joint pain. The study seems to show much better results for the SI joint fusion treated group than those patients who were randomized to be treated with physical therapy and SI joint injections. But after looking at the study, it’s really a lot more slight of hand than a study that shows SI joint fusion is the best thing since sliced bread. The study period reported is 6 months, however most patients won’t start suffering SI joint fusion side effects due to overload and advanced degeneration and destruction of the joints above and below (L5-S1 spine level and the hip joint) for 9-12 months. Hence, the downside side effects that makes fusing the SI joint a really dumb idea won’t show up in the time period that the study covered.
The upshot? Having seen many patients who have had SI joint fusions over the last 25 years, fusing this joint is a dumb idea. A 6 month study doesn’t tell us much, as the side effects will usually show up later. The study says that it will be run for 24 months, so maybe we’ll see other follow-up studies How the statistical guys handle “new” problems such as hip arthritis and degenerative disc disease at L5-S1 will be interesting. I bet you that these new pain problems caused by the SI joint fusion are considered to be just coincidental! There are so many regenerative medicine options for chronic SI joint pain from prolotherapy to PRP to stem cells, that injecting steroids to manage this pain syndrome is no longer a good idea. How would SI joint fusion compare to these treatments over a 1 or two year period? Right now nobody has that answer, but I can tell you we will continue to advise patients to avoid this surgery!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
